Lyme Disease
Lyme disease is the result of a bite by a tick and is associated with three different species of ticks. The clinical manifestations associated with Lyme disease are described as variable in severity as well as result in a diverse number of characteristics that affect a multitude of body systems.
The manifestations are divided into three key phases:
- Early Localized Disease
- Early Disseminated Disease
- Late Lyme Disease
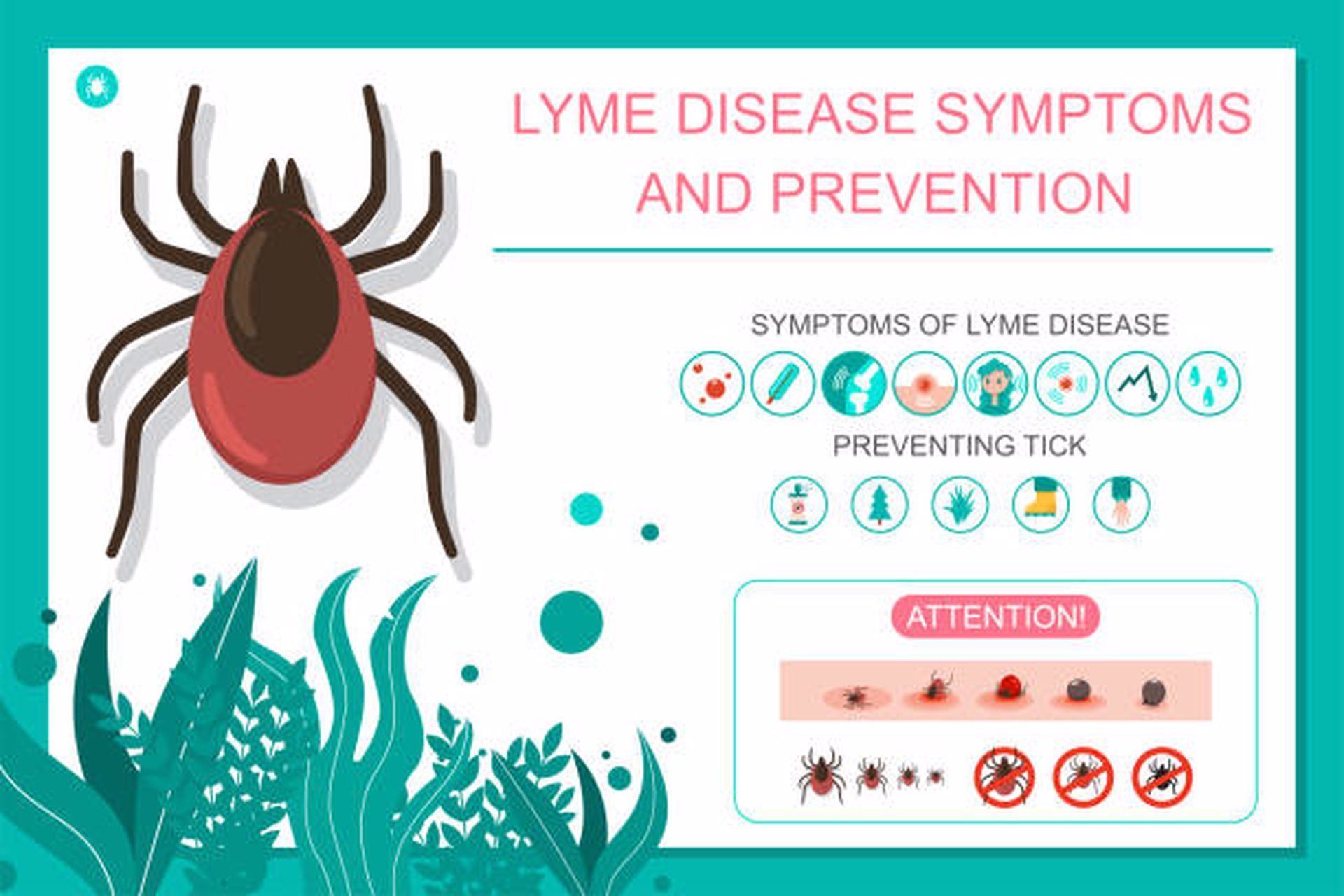
- Early localized disease is notable for the distinct skin lesion, erythema migrans which is typically apparent within a month from the initial bite. It is important to note that not all erythema migrans are the characteristic "bullseye" lesion but all have a notable amount of erythema and often vesicular lesions in the central portion of the lesion. The classic "bullseye" rash is notable for central clearing with a distinct spot of necrosis in the center of the lesion.
- Early disseminated disease characteristics include multiple erythema migrans lesions and cardiac and/or neurological findings. Cardiac findings are rare but may include heart block, cardiomyopathy, or pericarditis. Neurological findings are predominant and range from mild findings like headache to meningitis or nerve palsies. The highest reported manifestation involves the musculoskeletal system and include migratory arthralgias. Essentially any body system can be involved at this stage so the clinician should also be aware for involvement in the lymphatic system, liver, kidneys, as well as ocular findings.
- Late Lyme disease highlights the persistent arthralgias which can involve the large joints, particularly the knee joint, and other neurological findings such as encephalopathy or polyneuropathy. The timeline for the development of late Lyme disease is variable and can precipitate months to years following the acute infection.
Of note is the long-standing clinical symptoms that can persist following primary treatment for Lyme disease. Symptoms of fatigue, headache, cognitive strain, and arthritic pain may be reported for months following treatment and is called post-Lyme disease syndrome. This phenomenon can last for 6-12 months and the criteria for this syndrome includes confirmed diagnosis of Lyme disease, treatment with a recommended regimen, as well as persistent subjective symptoms (>6 months) despite therapy. Referral to a Lyme disease specialist is recommended to assess for complications like synovitis or neurological symptoms that interfere with quality of life or functionality. Additionally, it is not recommended to continue long-term antibiotic therapy in patients with post-Lyme disease syndrome and has been linked to increased mortality in some cases.
Diagnosis
The CDC has recently published new guidelines for diagnostic testing for Lyme disease and can be found by clicking here. Prior to testing the clinician should assess for the following to guide the need for diagnostic investigation: 1) Risk of exposure 2) Clinical manifestations as previously described that may indicate that the patient is experiencing symptoms from one of the three phases of disease. Testing is not recommended for patients that present with nonspecific symptoms or those that live in an endemic area which remain asymptomatic.
CDC currently recommends a two-step testing process for Lyme disease. Both steps are required and can be done using the same blood sample. If this first step is negative, no further testing is recommended. If the first step is positive or indeterminate (sometimes called “equivocal”), the second step should be performed. The overall result is positive only when the first test is positive (or equivocal) and the second test is positive (or for some tests equivocal).
Key points to remember
- Most Lyme disease tests are designed to detect antibodies made by the body in response to infection.
- Antibodies can take several weeks to develop, so patients may test negative if infected only recently.
- Antibodies normally persist in the blood for months or even years after the infection is gone; therefore, the test cannot be used to determine cure.
- Infection with other diseases, including some tickborne diseases, or some viral, bacterial, or autoimmune diseases, can result in false positive test results.
- Some tests give results for two types of antibody, IgM and IgG. Positive IgM results should be disregarded if the patient has been ill for more than 30 days.
Differential Diagnosis
- Chronic fatigue syndrome
- Fibromyalgia
- Myofascial pain syndrome
- Polymyalgia rheumatica
- Hypothyroidism
- Inflammatory myopathies
- Chronic traumatic encephalopathy
Treatment
For early Lyme disease, a short course of oral antibiotics such as doxycycline or amoxicillin is curative in the majority of the cases. In more complicated cases, Lyme disease can usually be successfully treated with three to four weeks of antibiotic therapy.
