Sex Cord-Stromal Tumors of the Testis - Departments of Pathology ...
Sex Cord-Stromal Tumors of the Testis - Departments of Pathology ...
Sex Cord-Stromal Tumors of the Testis - Departments of Pathology ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Sex</strong> <strong>Cord</strong>-<strong>Stromal</strong> <strong>Tumors</strong> <strong>of</strong> <strong>the</strong> <strong>Testis</strong><br />
Charles Zaloudek, M.D.<br />
Pr<strong>of</strong>essor, Department <strong>of</strong> <strong>Pathology</strong><br />
University <strong>of</strong> California, San Francisco<br />
505 Parnassus Ave., M563<br />
San Francisco, CA 94143<br />
Charles.zaloudek@ucsf.edu<br />
<strong>Sex</strong> cord stromal neoplasms are uncommon testicular tumors, accounting for only a<br />
few percent <strong>of</strong> all testicular tumors. These tumors occur over a wide age range, from children<br />
to <strong>the</strong> elderly. The clinical presentation is generally due to discovery <strong>of</strong> a testicular mass.<br />
Functional tumors are uncommon. The classification <strong>of</strong> testicular sex cord-stromal tumors is<br />
somewhat reminiscent <strong>of</strong> <strong>the</strong> classification <strong>of</strong> ovarian sex cord-stromal tumors, which are<br />
considerably more common. Thus, most pathologists are familiar with <strong>the</strong> terminology even<br />
though <strong>the</strong>y may have little experience with <strong>the</strong>se tumor types in <strong>the</strong> testis. We use <strong>the</strong> WHO<br />
classification, which is given below.<br />
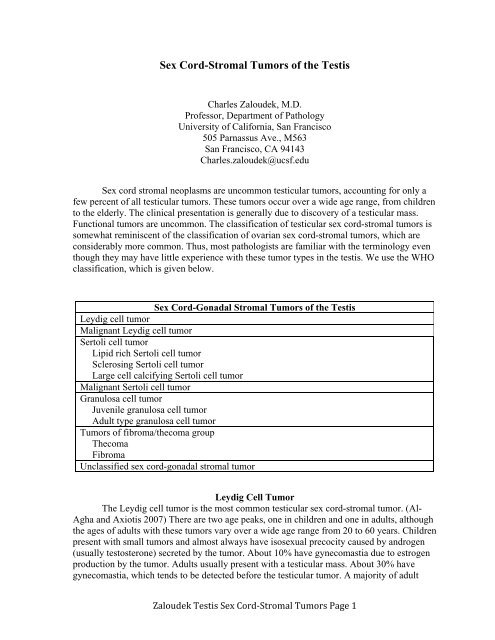
<strong>Sex</strong> <strong>Cord</strong>-Gonadal <strong>Stromal</strong> <strong>Tumors</strong> <strong>of</strong> <strong>the</strong> <strong>Testis</strong><br />
Leydig cell tumor<br />
Malignant Leydig cell tumor<br />
Sertoli cell tumor<br />
Lipid rich Sertoli cell tumor<br />
Sclerosing Sertoli cell tumor<br />
Large cell calcifying Sertoli cell tumor<br />
Malignant Sertoli cell tumor<br />
Granulosa cell tumor<br />
Juvenile granulosa cell tumor<br />
Adult type granulosa cell tumor<br />
<strong>Tumors</strong> <strong>of</strong> fibroma/<strong>the</strong>coma group<br />
Thecoma<br />
Fibroma<br />
Unclassified sex cord-gonadal stromal tumor<br />
Leydig Cell Tumor<br />
The Leydig cell tumor is <strong>the</strong> most common testicular sex cord-stromal tumor. (Al-<br />
Agha and Axiotis 2007) There are two age peaks, one in children and one in adults, although<br />
<strong>the</strong> ages <strong>of</strong> adults with <strong>the</strong>se tumors vary over a wide age range from 20 to 60 years. Children<br />
present with small tumors and almost always have isosexual precocity caused by androgen<br />
(usually testosterone) secreted by <strong>the</strong> tumor. About 10% have gynecomastia due to estrogen<br />
production by <strong>the</strong> tumor. Adults usually present with a testicular mass. About 30% have<br />
gynecomastia, which tends to be detected before <strong>the</strong> testicular tumor. A majority <strong>of</strong> adult<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 1
patients have abnormal serum levels <strong>of</strong> steroid hormones, with about a third <strong>of</strong> patients<br />
having increased serum androgens and a third, particularly those with gynecomastia, having<br />
elevated serum estrogen levels. (Suardi, Strada et al. 2009) Leydig cell tumors are more<br />
common in patients with cryptorchidism, testicular atrophy, and infertility. Some Leydig cell<br />
tumors occur in patients with germline fumarate hydratase mutations; (Carvajal-Carmona,<br />
Alam et al. 2006) <strong>the</strong>se patients are also predisposed to hereditary leiomyomatosis and renal<br />
cell carcinoma.<br />
Grossly, Leydig cell tumors are generally in <strong>the</strong> 2-5 cm range, with an average<br />
diameter <strong>of</strong> 3 cm. (Kim, Young et al. 1985) A few are larger, measuring up to 10 cm. On cut<br />
section, <strong>the</strong> testis contains a yellow, brown, or tan solid nodule. Many tumors have a<br />
characteristic yellow-brown color due to <strong>the</strong> presence <strong>of</strong> lip<strong>of</strong>uscin in <strong>the</strong> tumor cells.<br />
Hemorrhage and necrosis can be present. As would be anticipated, Leydig cell tumors are<br />
smaller in children. Leydig cell tumors are occasionally extratesticular. Gross features that<br />
are suggestive <strong>of</strong> malignancy include large size, an infiltrative edge, necrosis, and<br />
extratesticular extension. (Al-Agha and Axiotis 2007)<br />
Microscopically, <strong>the</strong> tumor cells grow mainly in sheets, but o<strong>the</strong>r patterns include<br />
pseudoglandular, trabecular, and nodular growth. (Kim, Young et al. 1985) The nodules are<br />
separated by fibrous stroma. At low magnification, some tumors appear circumscribed,<br />
o<strong>the</strong>rs push into <strong>the</strong> surrounding testicular parenchyma, and o<strong>the</strong>rs infiltrate <strong>the</strong> surrounding<br />
testis. Rare patterns include growth in cords and trabeculae, formation <strong>of</strong> vague follicles,<br />
microcystic growth, (Billings, Roth et al. 1999) which can be confused with yolk sac tumor,<br />
and a spindle cell pattern, which can be ei<strong>the</strong>r focal or be present extensively. (Ulbright,<br />
Srigley et al. 2002) In most tumors <strong>the</strong> cells are large and polygonal with abundant<br />
eosinophilic cytoplasm and round nuclei with prominent nucleoli. Some tumors contain large<br />
cells with abundant foamy pale cytoplasm and smaller nuclei resulting in an adrenal cortical<br />
like appearance, and in o<strong>the</strong>rs <strong>the</strong> cells have round hyperchromatic nuclei and less abundant<br />
cytoplasm. The nuclei tend to be relatively uniform and mitotic figures are usually<br />
infrequent. Finely granular yellow brown lip<strong>of</strong>uscin pigment is present in <strong>the</strong> tumor cell<br />
cytoplasm in some cases. Lip<strong>of</strong>uscin has a red purple granular appearance in sections stained<br />
with a PAS stain. Crystalloids <strong>of</strong> Reinke are eosinophilic rod-shaped cytoplasmic structures<br />
that are <strong>the</strong> most definitive light microscopic marker <strong>of</strong> Leydig cell differentiation.<br />
Unfortunately, <strong>the</strong>y can be identified in only about 40% <strong>of</strong> Leydig cell tumors. Rare Leydig<br />
cell tumors have clear cytoplasm, potentially leading to confusion with seminoma. Fat,<br />
calcifications, and osseous metaplasia sometimes present. (Ulbright, Srigley et al. 2002)<br />
Often, <strong>the</strong> fat appears to result from accumulation <strong>of</strong> lipid in <strong>the</strong> tumor cells.<br />
Immunohistochemistry is useful in <strong>the</strong> diagnosis <strong>of</strong> Leydig cell tumors. Positive<br />
markers include inhibin, calretinin, and melan-A. (Busam, Iversen et al. 1998; Iczkowski,<br />
Bostwick et al. 1998; McCluggage, Shanks et al. 1998; Augusto, Leteurtre et al. 2002) We<br />
have had good luck staining Leydig cell tumors with steroidogenic factor-1. CD99 is<br />
positive, with staining <strong>of</strong> tumor cell membranes in about 2/3 <strong>of</strong> cases. Most Leydig cell<br />
tumors show positive staining for vimentin. O<strong>the</strong>r staining reactions that have been reported<br />
include staining for chromogranin (>90%), synaptophysin (70%), S100 (8% in one study,<br />
62% in ano<strong>the</strong>r) and cytokeratin (~ 40%). (Iczkowski, Bostwick et al. 1998)<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 2
UCSF Immunostain Panel for Leydig Cell Tumor<br />
Stain Anticipated Result<br />
Inhibin Positive, cytoplasmic<br />
Steroidogenic factor-1 Positive, nuclear<br />
Melan-A Positive, cytoplasmic, granular<br />
Cytokeratin cocktail Negative (but 30-40% positive)<br />
Epi<strong>the</strong>lial Membrane Antigen Negative<br />
Malignant Leydig cell tumors are most common in older patients. (Cheville, Sebo et<br />
al. 1998) <strong>Tumors</strong> that occur in patients with gynecomastia are more likely to be benign. No<br />
clinically malignant Leydig cell tumors have occurred in prepuberal children, although one<br />
tumor in a 1-year-old boy appeared histologically malignant. (Drut, Wludarski et al. 2006)<br />
Pathologic features that are suspicious for malignancy include large tumor size (> 5cm),<br />
frequent mitotic figures (> 3/10 hpf), atypical mitotic figures, vascular space invasion,<br />
nuclear atypia, necrosis, invasive borders, and invasion <strong>of</strong> <strong>the</strong> rete testis or beyond. (Kim,<br />
Young et al. 1985; Cheville, Sebo et al. 1998) Clinicopathological studies based on<br />
consultation cases seem to have a higher percentage <strong>of</strong> malignant tumors than actually occur<br />
in practice. Several recent clinical series have found tumor related deaths to be uncommon (1<br />
<strong>of</strong> 52 patients in one study; 0 <strong>of</strong> 37patients in ano<strong>the</strong>r). (Di Tonno, Tavolini et al. 2009;<br />
Suardi, Strada et al. 2009) <strong>Testis</strong> sparing surgery appears safe and effective, provided that <strong>the</strong><br />
diagnosis can be made at frozen section and <strong>the</strong> tumor is small with no gross or histologic<br />
features <strong>of</strong> suggestive <strong>of</strong> malignancy. (Giannarini, Mogorovich et al. 2007; Suardi, Strada et<br />
al. 2009) No effective chemo<strong>the</strong>rapy protocols have been identified nor does radiation<br />
<strong>the</strong>rapy appear helpful. It is unclear whe<strong>the</strong>r retroperitoneal lymph node dissection is<br />
beneficial.<br />
Features Suggestive <strong>of</strong> Malignancy in Leydig Cell <strong>Tumors</strong><br />
Old age (never malignant in young children)<br />
Large size, tumor diameter > 5 cm<br />
Mitotic activity (> 3 mf per 10 hpf)<br />
Atypical mitotic figures<br />
Lymphovascular space invasion<br />
Nuclear atypia<br />
Necrosis<br />
Invasive growth<br />
The differential diagnosis <strong>of</strong> a Leydig cell tumor includes a number <strong>of</strong> non-neoplastic<br />
hyperplasias as well as several types <strong>of</strong> neoplasms.<br />
-Leydig cell hyperplasia, nodular type. Hyperplastic Leydig cell nodules exhibit nondestructive<br />
growth <strong>of</strong> Leydig cells in an interstitial location between <strong>the</strong> tubules. The nodules<br />
tend to be multiple, and <strong>the</strong>y can be bilateral. They are usually small (< 0.5 cm). Leydig cell<br />
hyperplasia can occur in patients with elevated gonadotropin levels.<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 3
-Testicular tumor <strong>of</strong> <strong>the</strong> adrenogenital syndrome (TTAGS). Patients with adrenogenital<br />
syndrome, usually <strong>of</strong> <strong>the</strong> salt loosing type caused by a 21-hydroxylase deficiency, or<br />
Nelson’s syndrome (ACTH secreting pituitary adenoma in patients treated by bilateral<br />
adrenalectomy for Cushing’s syndrome) can have multifocal and bilateral nodules that can<br />
mimic a Leydig cell tumor. (Rutgers, Young et al. 1988) TTAGS are hyperplastic nodules<br />
caused by elevated levels <strong>of</strong> ACTH. Often, <strong>the</strong> history is known, which facilitates <strong>the</strong> correct<br />
diagnosis, but occasionally <strong>the</strong> testicular tumors are discovered prior to diagnosis <strong>of</strong> <strong>the</strong><br />
adrenogenital syndrome. Grossly, <strong>the</strong> tumors can be large, measuring up to 5-10 cm, or <strong>the</strong>y<br />
can be small and impalpable. Small tumors are <strong>of</strong>ten centered in <strong>the</strong> hilum <strong>of</strong> <strong>the</strong> testis. In<br />
general, tumors in children are small and those that are detected in older patients are larger.<br />
The cut surfaces are brown with confluent nodules separated by broad bands <strong>of</strong> fibrous<br />
tissue. The tumor cells are large and polygonal with uniform round nuclei with nucleoli and<br />
abundant eosinophilic or pale cytoplasm. Some nodules contain cells with clear vacuolated<br />
cytoplasm. The cytoplasm contains lip<strong>of</strong>uscin but no Reinke crystalloids are present. Fibrous<br />
bands that are generally broader and more extensive than occur in Leydig cell tumors<br />
separate nests <strong>of</strong> cells. Sometimes, when <strong>the</strong> nodules are hilar, rete tubules are present<br />
between <strong>the</strong>m. These “tumors” are not true neoplasms, but nodular hyperplasias that regress<br />
with treatment that lowers adrenocorticotrophin levels.<br />
-Large cell calcifying Sertoli cell tumor. Many examples <strong>of</strong> this tumor occur in patients with<br />
<strong>the</strong> Carney syndrome, as discussed below. These tumors can be confused with Leydig cell<br />
tumors because <strong>the</strong> tumor cells are polygonal and have abundant eosinophilic cytoplasm. No<br />
Reinke crystalloids are identified. This type <strong>of</strong> Sertoli cell tumor characteristically contains<br />
calcifications, can grow in tubules, and has a more myxoid stroma that <strong>of</strong>ten contains<br />
neutrophils.<br />
-Seminoma. A Leydig cell tumor with clear cytoplasm can be confused with a seminoma, but<br />
in <strong>the</strong> case <strong>of</strong> <strong>the</strong> Leydig cell tumor <strong>the</strong> clear cytoplasm due to <strong>the</strong> presence <strong>of</strong> lipids, not<br />
glycogen. Findings that are present in association with seminoma, but not a Leydig cell<br />
tumor, include intratubular germ cell neoplasia, lymphocytes, typically in fibrous septae and<br />
sometimes forming germinal centers, and granulomas. Of course, <strong>the</strong> immunohistochemical<br />
features <strong>of</strong> a seminoma are totally different than those <strong>of</strong> a Leydig cell tumor.<br />
Sertoli Cell Tumor<br />
A variety <strong>of</strong> types <strong>of</strong> Sertoli cell tumor have been described, with interesting<br />
histologic patterns or unusual clinical associations, or both. Sertoli cell tumors, nos are <strong>the</strong><br />
most common, and a tumor designated simply as a “Sertoli cell tumor” is generally taken to<br />
be a Sertoli cell tumor, nos.<br />
Sertoli Cell <strong>Tumors</strong> <strong>of</strong> <strong>the</strong> <strong>Testis</strong><br />
Sertoli cell tumor, nos<br />
Sclerosing Sertoli cell tumor<br />
Large cell calcifying Sertoli cell tumor<br />
Sertoli cell tumor associated with Peutz-Jeghers syndrome<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 4
Sertoli cell tumors occur in patients <strong>of</strong> all ages. About a third <strong>of</strong> <strong>the</strong>m occur in<br />
children less than 10 years old, (Harms and Kock 1997) but <strong>the</strong>y are most common in<br />
middle-aged men. The average age is about 45. (Young, Koelliker et al. 1998) The typical<br />
presentation is with a slowly enlarging testicular mass. They are almost always unilateral.<br />
Most tumors are nonfunctional. <strong>Tumors</strong> that secret estrogens are unusual, but <strong>the</strong>se can cause<br />
gynecomastia or impotence.<br />
Gynecomastia in Sertoli Cell <strong>Tumors</strong><br />
Sertoli cell tumor, nos Rare<br />
Sclerosing Sertoli cell tumor Never<br />
Large cell calcifying Sertoli cell tumor Rare<br />
Grossly, Sertoli cell tumors are solid gray, white or tan masses, usually less than 4 cm<br />
in diameter. Cystic change can be present.<br />
Microscopically, a nodular pattern is <strong>of</strong>ten prominent at low magnification, with <strong>the</strong><br />
nodules separated by broad bands <strong>of</strong> fibrous tissue. A variety <strong>of</strong> growth patterns are<br />
recognized, including growth <strong>of</strong> tumor cells in sheets, nests, trabeculae and cords. However,<br />
<strong>the</strong>se patterns are not specific and for a definitive diagnosis tubules must be identified. The<br />
tubules can be solid or hollow and rarely elongated branching rete like tubules lined by<br />
cuboidal cells are present. The tubules are <strong>of</strong>ten poorly formed and sometimes it requires<br />
some imagination to recognize <strong>the</strong>m. The background tends to be fibrous but it can be<br />
hyalinized or myxoid. The tumor cells are cuboidal to columnar and have scant to moderate<br />
pale or clear cytoplasm. Some tumors are composed mainly <strong>of</strong> polygonal cells with abundant<br />
eosinophilic cytoplasm. Zones composed <strong>of</strong> spindle cells are occasionally present in a Sertoli<br />
cell tumor. A variant with abundant clear foamy cytoplasm, <strong>the</strong> lipid rich variant, has been<br />
described. Cytoplasmic vacuoles are common and prominent cytoplasmic vacuolization can<br />
result in a microcystic appearance. The tumor cell nuclei are uniform and round to oval with<br />
small nucleoli.<br />
Immunohistochemical stains for inhibin, cytokeratin, and vimentin are positive.<br />
(Iczkowski, Bostwick et al. 1998; McCluggage, Shanks et al. 1998; Kommoss, Oliva et al.<br />
2000; Kato, Fukase et al. 2001; Comperat, Tissier et al. 2004) About half stain for calretinin.<br />
O<strong>the</strong>r sex cord-stromal markers, such as WT-1, CD99 and melan-A can be positive. Many<br />
Sertoli cell tumors show positive staining for S100. Chromogranin and synaptophysin have<br />
been reported as positive in some studies. Sertoli cells are usually negative for EMA, but<br />
malignant Sertoli cell tumors can be positive.<br />
About 10% <strong>of</strong> Sertoli cell tumors are malignant. Malignant Sertoli cell tumors occur<br />
in children as well as in adults. Gynecomastia is more common in malignant cases.<br />
Malignant Sertoli cell tumors do not respond to chemo<strong>the</strong>rapy or radio<strong>the</strong>rapy, so surgery is<br />
<strong>the</strong> mainstay <strong>of</strong> treatment and retroperitoneal lymph node dissection is generally advised.<br />
Metastatic spread is to <strong>the</strong> retroperitoneal lymph nodes and lungs. Pathologic features that<br />
suggest malignancy include marked nuclear atypia and pleomorphism, frequent mitotic<br />
figures (> 5mf/10hpf), vascular invasion, necrosis, large size (>5 cm), and predominance <strong>of</strong> a<br />
diffuse growth pattern.<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 5
Several benign pseudotumors must be considered in <strong>the</strong> differential diagnosis, along<br />
with o<strong>the</strong>r neoplasms. The differential diagnosis is mainly with <strong>the</strong> following:<br />
-Hamartomatous Sertoli cell nodules <strong>of</strong> <strong>the</strong> androgen insensitivity syndrome. Patients with<br />
<strong>the</strong> AIS (“testicular feminization”) have multiple testicular hamartomatous nodules<br />
composed <strong>of</strong> tubules lined by Sertoli cells. Leydig cells are <strong>of</strong>ten present in <strong>the</strong> stroma<br />
between <strong>the</strong> tubules, in contrast to Sertoli cell tumors, where Leydig cells are pushed aside.<br />
About 25% <strong>of</strong> patients with <strong>the</strong> AIS develop multifocal bilateral Sertoli cell adenomas<br />
composed <strong>of</strong> pure proliferations <strong>of</strong> Sertoli cells lining tubules. It is unclear whe<strong>the</strong>r <strong>the</strong>se are<br />
hyperplastic nodules, or autonomous neoplastic nodules but in any event malignant behavior<br />
has never been observed. The adenomas <strong>of</strong>ten contain eosinophilic waxy basement<br />
membrane deposits.<br />
-Small Sertoli cell nodules. Small nodules <strong>of</strong> Sertoli cells are a common incidental<br />
microscopic finding common in orchiectomy specimens from cryptorchid patients. These<br />
nodules are not grossly visible, in contrast to Sertoli cell tumors, which are usually > 1 cm in<br />
diameter. The nodules <strong>of</strong>ten contain central accumulations <strong>of</strong> basement membrane material.<br />
-Seminoma. In some malignant Sertoli cell tumors <strong>the</strong> tumor cells have clear cytoplasm and<br />
grow in sheets. Lymphocytes are scattered among <strong>the</strong> tumor cells, but plasma cells, which<br />
are uncommon in seminoma, are <strong>of</strong>ten numerous as well. This results in a histologic picture<br />
that can lead to a misdiagnosis as seminoma. (Henley, Young et al. 2002; Ulbright 2008)<br />
Unlike seminoma cells, <strong>the</strong> Sertoli cells <strong>of</strong>ten contain cytoplasmic vacuoles, have smaller<br />
round nuclei, and do not have conspicuous nucleoli. Mitotic figures are usually more<br />
numerous in seminoma. The presence <strong>of</strong> granulomas or intratubular germ cell neoplasia<br />
would favor a diagnosis <strong>of</strong> seminoma. The immunohistochemical findings permit a clear<br />
distinction between Sertoli cell tumor and seminoma. Many seminoma-like Sertoli cell<br />
tumors occur in older men at an age when seminoma is uncommon (> 55 years old).<br />
Variants <strong>of</strong> Sertoli Cell Tumor<br />
Several variants <strong>of</strong> Sertoli cell tumor have been described. These have distinctive<br />
histologic or clinical features, or both. The most important <strong>of</strong> <strong>the</strong>se are sclerosing Sertoli cell<br />
tumor, large cell calcifying Sertoli cell tumor and Sertoli cell tumors in patients with <strong>the</strong><br />
Peutz-Jeghers syndrome.<br />
Sclerosing Sertoli Cell Tumor<br />
Sclerosing Sertoli cell tumors occur predominantly in young men with an average age<br />
<strong>of</strong> 35 years. (Zukerberg, Young et al. 1991) They ei<strong>the</strong>r present as a painless slowly<br />
enlarging testicular mass without any associated hormonal symptoms or <strong>the</strong> tumor is<br />
incidental finding.Grossly, sclerosing Sertoli cell tumors are small hard solid nodules with a<br />
white to yellow tan cut surface. Most are < 1.5 cm in diameter, although rare larger tumors<br />
have been reported. Microscopically, <strong>the</strong> tumor cells grow in cords, solid or hollow tubules,<br />
or as nests <strong>of</strong> cells. The key finding in this variant <strong>of</strong> Sertoli cell tumor is <strong>the</strong> densely<br />
collagenous background stroma that dominates <strong>the</strong> histologic picture and compresses <strong>the</strong><br />
tubules, prompting <strong>the</strong> name “sclerosing” Sertoli cell tumor. (Zukerberg, Young et al. 1991)<br />
The sclerosis should be present throughout <strong>the</strong> tumor, not just focally, for classification as a<br />
sclerosing Sertoli cell tumor. The tumor cells nuclei vary from large and vesicular to small<br />
and hyperchromatic. They are usually columnar or cuboidal and have pale, sometimes<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 6
vacuolated cytoplasm. Mitotic activity and nuclear atypia have only een reported in one case.<br />
All reported sclerosing Sertoli cell tumors have had a benign evolution.<br />
Large Cell Calcifying Sertoli Cell Tumor<br />
Patients with this type <strong>of</strong> Sertoli cell tumor tend to be young, with an average age <strong>of</strong><br />
16, although tumors occur over a wide age range from children to older adults. (Proppe and<br />
Scully 1980) The usual presentation is with a slowly enlarging painless testicular mass.<br />
Hormones may be produced by <strong>the</strong> tumor or by hyperplastic Leydig cells in <strong>the</strong> surrounding<br />
testis, and some patients accordingly present with endocrine associated symptoms such as<br />
gynecomastia or isosexual precocity. About 40% <strong>of</strong> large cell calcifying Sertoli cell tumors<br />
occur in patients with Carney’s syndrome or ano<strong>the</strong>r genetic syndrome such as Peutz-Jeghers<br />
syndrome. (Kratzer, Ulbright et al. 1997) <strong>Tumors</strong> in Carney’s patients are small, bilateral and<br />
multifocal and <strong>the</strong>y are usually detected in childhood or adolescence. O<strong>the</strong>r findings<br />
associated with <strong>the</strong> Carney syndrome include lentigines <strong>of</strong> <strong>the</strong> face, myxomas <strong>of</strong> <strong>the</strong> heart,<br />
skin and s<strong>of</strong>t tissue, myxoid fibroadenomas <strong>of</strong> <strong>the</strong> breast, blue nevi <strong>of</strong> skin, pigmented<br />
nodules <strong>of</strong> <strong>the</strong> adrenal cortex with Cushing’s syndrome, human growth hormone producing<br />
adenomas <strong>of</strong> pituitary and psammomatous melanotic schwannomas. Pathologists should<br />
always bring up <strong>the</strong> possibility that <strong>the</strong> patient might have <strong>the</strong> Carney syndrome if a large cell<br />
calcifying Sertoli cell tumor is diagnosed, particularly if it is bilateral and multifocal.<br />
Grossly, <strong>the</strong> tumor is tan or yellow and contains gritty areas <strong>of</strong> calcification. Most measure<br />
less than 4 cm in diameter. Large cell calcifying Sertoli cell tumors are unusual in that <strong>the</strong>y<br />
can be multifocal and about 40% are bilateral.<br />
Microscopically, <strong>the</strong> tumor consists <strong>of</strong> nests, cords, trabeculae and solid tubules <strong>of</strong><br />
polygonal cells with abundant eosinophilic cytoplasm. The tumor cell nuclei are round and<br />
vesicular with prominent nucleoli. Mitotic figures are rare. Intratubular growth and<br />
calcifications are common. The tumor cells grow in myxoid to collagenous stroma that is<br />
calcified or ossified in about half <strong>the</strong> cases. A neutrophilic stromal infiltrate is characteristic.<br />
The tumor cells stain for vimentin and are inhibin and melan-A positive. (Petersson,<br />
Bulimbasic et al. 2010) They are usually cytokeratin negative although infrequently <strong>the</strong>re is<br />
minimal focal staining. (Kratzer, Ulbright et al. 1997) The tumor cells are EMA negative.<br />
Given <strong>the</strong> appearance <strong>of</strong> <strong>the</strong> tumor cells, it is worth noting that <strong>the</strong>y usually stain for S100,<br />
which could potentially lead to confusion with metastatic melanoma.<br />
The differential diagnosis includes Leydig cell tumor because <strong>of</strong> <strong>the</strong> polygonal cell<br />
shape and abundant eosinophilic cytoplasm, but Leydig cell tumors generally lack a<br />
neutrophilic infiltrate and calcifications, do not exhibit tubular growth and do not grow<br />
within tubules. Large cell calcifiying Sertoli cell tumors do not contain crystalloids <strong>of</strong> Reinke<br />
or lip<strong>of</strong>uscin.<br />
Malignant large cell calcifying Sertoli cell tumors are rare, but some have been<br />
reported. (Kratzer, Ulbright et al. 1997) Patients with malignant tumors are older than those<br />
with malignant tumors (average age 39 vs 17) and malignant tumors generally do not occur<br />
in patients with <strong>the</strong> Carney syndrome. Features suggestive <strong>of</strong> malignancy include large size<br />
(>4 cm), extratesticular growth, tumor cell necrosis, high-grade nuclear atypia, frequent<br />
mitotic figures (mitotic rate > 3 mf/10 hpf) and vascular invasion. It has been suggested that<br />
if one <strong>of</strong> <strong>the</strong>se features is present <strong>the</strong> possibility <strong>of</strong> malignancy should be mentioned, and if<br />
two or more are present <strong>the</strong> tumor should be classified as malignant. (Kratzer, Ulbright et al.<br />
1997) Invasion <strong>of</strong> <strong>the</strong> rete testis has been noted in a few benign cases. (Plata, Algaba et al.<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 7
1995) Occasional tumors with none <strong>of</strong> <strong>the</strong>se features, such as one with minimal atypia and no<br />
mitotic activity but with invasion <strong>of</strong> <strong>the</strong> rete testis, prove to be malignant. (De Raeve,<br />
Schoonooghe et al. 2003)<br />
Sertoli Cell Proliferations in Peutz Jeghers Syndrome<br />
Patients with <strong>the</strong> Peutz-Jeghers syndrome develop multifocal bilateral intratubular<br />
proliferations <strong>of</strong> Sertoli cells that occur in lobular clusters through out <strong>the</strong> parenchyma.<br />
(Venara, Rey et al. 2001; Ulbright, Amin et al. 2007) Most patients are children; <strong>the</strong>y all<br />
have gynecomastia and some have isosexual precocity depending on <strong>the</strong> hormone or<br />
hormones produced. Many patients have o<strong>the</strong>r features <strong>of</strong> Peutz-Jeghers syndrome, such as<br />
pigmented macules around <strong>the</strong> mouth and on <strong>the</strong> lips. The testes are generally bilaterally<br />
enlarged with echogenic foci on ultrasound examination, but a palpable mass is not present;<br />
rare patients have unilateral testicular enlargement. The diagnosis is generally made by<br />
testicular biopsy, usually performed bilaterally. The involved tubules are expanded and<br />
contain cells similar to those in a large cell calcifying Sertoli tumor. They are polygonal with<br />
abundant eosinophilic cytoplasm. There is abundant eosinophilic hyalinized basement<br />
membrane material in <strong>the</strong> expanded tubules. Sometimes <strong>the</strong> growth pattern is annular and<br />
with <strong>the</strong> prominent hyaline material it is reminiscent <strong>of</strong> <strong>the</strong> sex cord tumor with annular<br />
tubules (SCTAT) that occurs in <strong>the</strong> ovaries <strong>of</strong> women with <strong>the</strong> Peutz-Jeghers syndrome.<br />
Usually, calcifications are not present. In most cases <strong>the</strong> proliferation is entirely intratubular,<br />
but in a minority <strong>of</strong> patients an invasive Sertoli cell tumor is also present. (Young,<br />
Gooneratne et al. 1995; Venara, Rey et al. 2001) The invasive tumors are usually small and<br />
<strong>the</strong>ir classification is problematic. Some resemble large cell calcifying Sertoli cell tumors but<br />
<strong>the</strong>y lack calcifications and do not have <strong>the</strong> prominent fibromyxoid stroma with neutrophils.<br />
O<strong>the</strong>rs have a more tubular pattern. Followup has not revealed progression in patients who<br />
have only intratubular proliferations at diagnosis, so <strong>the</strong> nature <strong>of</strong> <strong>the</strong>se proliferations<br />
remains unsettled. Ulbright et al favor interpreting <strong>the</strong>m as intratubular neoplasms because <strong>of</strong><br />
<strong>the</strong> occasional association with an invasive neoplasm.<br />
Granulosa Cell Tumor<br />
Granulosa cell tumors are rare types <strong>of</strong> testicular tumors. There are two variants,<br />
similar to <strong>the</strong> situation in <strong>the</strong> ovary. One type occurs mainly in adults, and is termed <strong>the</strong> adult<br />
type granulosa cell tumor. The o<strong>the</strong>r type occurs predominantly in young children, and is<br />
termed <strong>the</strong> juvenile type <strong>of</strong> granulosa cell tumor.<br />
Adult Granulosa Cell Tumor<br />
Adult type granulosa cell tumors are very rare. (Nistal, L†zaro et al. 1992; Jimenez-<br />
Quintero, Ro et al. 1993) In <strong>the</strong> only series reported, 7 granulosa cell tumors were found in a<br />
review <strong>of</strong> 52 sex cord stromal tumors at MD Anderson. (Jimenez-Quintero, Ro et al. 1993)<br />
Six cases were pathology consultations and one was a patient treated at MD Anderson. They<br />
occur over a wide age range, from 16-76 years. The average age is in <strong>the</strong> mid 40’s. The<br />
presentation is with a painless testicular mass. A significant number <strong>of</strong> tumors have been<br />
asymptomatic and detected during routine physical examinations. Many tumors are<br />
nonfunctional, but o<strong>the</strong>rs secrete estrogen and cause gynecomastia.<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 8
Grossly, adult type granulosa cell tumors can be solid, cystic, or solid and cystic.<br />
They form well-circumscribed nodules with cut surfaces that are yellow to gray. The average<br />
size is about 5 cm.<br />
The same microscopic patterns that are seen in ovarian granulosa cell tumors occur in<br />
testicular granulosa cell tumors. These include micr<strong>of</strong>ollicular, trabecular, gyriform, insular,<br />
and diffuse patterns <strong>of</strong> growth. The diffuse pattern is <strong>the</strong> most common one. The tumor cells<br />
have scant pale cytoplasm. The nuclei are pale and round to oval with small nucleoli and,<br />
sometimes, nuclear grooves. Mitotic figures are usually uncommon, but <strong>the</strong>y are occasionally<br />
numerous and readily identified.<br />
Granulosa cell tumors <strong>of</strong> <strong>the</strong> testis show positive immunohistochemical staining for<br />
inhibin, vimentin, and, in some tumors, cytokeratin. Staining for EMA is negative.<br />
Most <strong>of</strong> <strong>the</strong> reported cases have been clinically benign. The largest series included<br />
only seven patients, but 2 <strong>of</strong> <strong>the</strong> 5 patients included in that series developed metastases,<br />
(Jimenez-Quintero, Ro et al. 1993) and o<strong>the</strong>r patients with malignant tumors have been<br />
reported. The diagnosis in some reported cases is questionable; for example, Hammerich et al<br />
reported a tumor as a granulosa cell tumor, but <strong>the</strong>ir illustrations show a tumor that contains<br />
closed and open tubules, more suggestive <strong>of</strong> a Sertoli cell tumor. (Hammerich, Hille et al.<br />
2008) Features that are worrisome for malignancy include large tumor size, vascular<br />
invasion, hemorrhage, and necrosis.<br />
Juvenile Granulosa Cell Tumor<br />
Juvenile granulosa cell tumors <strong>of</strong> <strong>the</strong> testis occur almost exclusively in young<br />
children. In <strong>the</strong> Kiel pediatric tumor registry sex cord-stromal tumors accounted for 17.7% <strong>of</strong><br />
all testicular tumors, with juvenile granulosa cell tumors constituting 31.4% <strong>of</strong> <strong>the</strong> total.<br />
(Harms and Kock 1997) A majority <strong>of</strong> <strong>the</strong>se tumors are diagnosed during <strong>the</strong> first days or<br />
weeks <strong>of</strong> life, (Lawrence, Young et al. 1985) and presumably are congenital tumors. More<br />
than 95% are diagnosed before <strong>the</strong> patient has reached <strong>the</strong> age <strong>of</strong> 1 year. As might be<br />
anticipated, some cases are diagnosed antenatally. (Peterson and Skoog 2008) Almost all<br />
patients present with a painless scrotal mass, but a few present because <strong>of</strong> testicular torsion.<br />
(Nistal, Redondo et al. 1988) A few tumors have been reported to occur in undescended<br />
testicles. Hormonal symptoms almost never occur. Most patients have a normal 46XY<br />
karyotype.<br />
On gross exam, <strong>the</strong> testis contains a solid to cystic gray or yellow nodule that usually<br />
occupies most <strong>of</strong> <strong>the</strong> testis, <strong>of</strong>ten leaving only a thin rim <strong>of</strong> normal testicular parenchyma.<br />
The cut surface can be nodular or microcystic, with small cysts only 1-2 mm in diameter, or<br />
larger cysts may be present. The tumor size ranges from less than a cm to about 5 cm, with<br />
an average diameter <strong>of</strong> about 2 cm. (Lawrence, Young et al. 1985; Harms and Kock 1997)<br />
Microscopically, solid cellular areas are intermixed with follicle like structures filled<br />
with mucoid material. The follicle contents are <strong>of</strong>ten basophilic and stain lightly with<br />
mucicarmine. The follicles tend to be large and somewhat irregular, and can be termed<br />
macr<strong>of</strong>ollicles. The follicles are lined by several layers <strong>of</strong> stratified tumor cells and<br />
surrounded by a spindle cell stroma or by neoplastic granulosa cells. Solid areas may contain<br />
abundant hyalinized stroma. The tumor cells have abundant pale to eosinophilic cytoplasm<br />
and in some tumors <strong>the</strong>y are focally or diffusely luteinized. The nuclei are round and<br />
hyperchromatic and <strong>of</strong>ten contain conspicuous nucleoli. Mitotic figures are generally readily<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 9
identified and <strong>the</strong>y can be numerous. The degree <strong>of</strong> atypia is typically less than is seen in<br />
ovarian juvenile granulosa cell tumors.<br />
Immunohistochemical studies <strong>of</strong> <strong>the</strong>se tumors are limited, but <strong>the</strong>y have been shown<br />
to be positive for inhibin, vimentin and CD99 and to stain focally for cytokeratin. As has<br />
been observed in ovarian granulosa cell tumors, <strong>the</strong> cells can stain for S100 and SMA.<br />
(Alexiev, Alaish et al. 2007) The results <strong>of</strong> staining for o<strong>the</strong>r antigens have not been reported,<br />
but positive staining for sex cord-stromal markers such as calretinin and steroidogenic factor-<br />
1 is likely to be present.<br />
Malignant behavior has not reported. Follow-up studies are limited, but all patients<br />
have been well after orchiectomy or enucleation. In view <strong>of</strong> <strong>the</strong> favorable outcome, fertility<br />
sparing enucleation has been advocated in patients who have a normal serum AFP<br />
(presumably excluding yolk sac tumor). (Shukla, Huff et al. 2004)<br />
The histogenesis is controversial. In one series <strong>of</strong> 14 juvenile granulosa cell tumors<br />
one example showed intratubular growth adjacent to <strong>the</strong> main tumor mass. This has led to<br />
speculation that <strong>the</strong> tumors may be derived from Sertoli cells.<br />
The differential diagnosis includes o<strong>the</strong>r types <strong>of</strong> sex cord stromal tumors, but <strong>the</strong><br />
main differential diagnosis is with yolk sac tumor. Yolk sac tumor exhibits a number <strong>of</strong><br />
distinctive growth patterns that are not seen in juvenile granulosa cell tumor, so adequate<br />
histologic study usually resolves <strong>the</strong> issue. In addition, <strong>the</strong>re are significant<br />
immunohistochemical differences between <strong>the</strong> two, with juvenile granulosa cell tumor being<br />
positive for inhibin, calretinin, and steroidogenic factor-1, and yolk sac tumor showing<br />
positive staining for cytokeratin, alpha-fetoprotein, SALL4, and glypican-3.<br />
Fibroma Thecoma Group<br />
<strong>Tumors</strong> that resemble fibromas or <strong>the</strong>comas <strong>of</strong> <strong>the</strong> ovary are extremely rare. (Jones,<br />
Young et al. 1997) They are generally small and circumscribed with a yellow or white cut<br />
surface. Microscopically, <strong>the</strong>y consist <strong>of</strong> bundles <strong>of</strong> bland spindle cells with oval nuclei and<br />
scanty cytoplasm. A variable amount <strong>of</strong> collagen is present in <strong>the</strong> background. Several<br />
cellular fibromas, similar in appearance to <strong>the</strong> corresponding ovarian tumors, have been<br />
reported. Several tumors with minor aggregates <strong>of</strong> sex cord elements have been reported. (De<br />
Pinieux, Glaser et al. 1999) The presence <strong>of</strong> more than a minor amount <strong>of</strong> sex cord cells<br />
excludes a tumor from <strong>the</strong> fibroma category, and requires its placement in <strong>the</strong> mixed or<br />
unclassified category, discussed below, since such tumors have metastatic potential that is<br />
lacking in fibroma.<br />
Mixed and Unclassified <strong>Sex</strong> <strong>Cord</strong> <strong>Stromal</strong> <strong>Tumors</strong><br />
This category contains tumors that cannot be accurately placed into one <strong>of</strong> <strong>the</strong> defined<br />
categories <strong>of</strong> sex cord stromal tumors. They usually present as a painless testicular mass.<br />
About a third <strong>of</strong> <strong>the</strong>se tumors occur in children, in whom 2/3 <strong>of</strong> sex cord stromal tumors fall<br />
into this category. About 15% <strong>of</strong> patients have gynecomastia.<br />
Grossly, <strong>the</strong>y are gray, tan or yellow solid nodules. Microscopically, <strong>the</strong>y <strong>of</strong>ten<br />
contain a mixture <strong>of</strong> sex cord and stromal elements. A combination <strong>of</strong> epi<strong>the</strong>lioid and<br />
spindled tumor cells is typical, although in some tumors spindled cells predominate.<br />
(Renshaw, Gordon et al. 1997; Magro, Gurrera et al. 2007) In some tumors <strong>the</strong>re are focal<br />
Sertoli tubules or aggregates <strong>of</strong> granulosa like cells, but <strong>the</strong> tumor does not fit well into ei<strong>the</strong>r<br />
category. In tumors that contain a mixture <strong>of</strong> well defined types <strong>of</strong> sex cord and stromal<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 10
elements, all should be listed in <strong>the</strong> report; <strong>the</strong> behavior is likely to be determined by a<br />
combination <strong>of</strong> <strong>the</strong> percentage <strong>of</strong> each type and its malignant potential.<br />
These tumors have all been benign in children less than 10 years <strong>of</strong> age but about 20% <strong>of</strong><br />
those that occur in older patients are malignant. Worrisome findings include cellular atypia<br />
and pleomorphism, a high mitotic rate, necrosis, vascular invasion, an invasive margin and<br />
large tumor size.<br />
References<br />
Al-Agha, O. M. and C. A. Axiotis (2007). "An in-depth look at Leydig cell tumor <strong>of</strong> <strong>the</strong> testis." Arch Pathol<br />
Lab Med 131(2): 311-317.<br />
Alexiev, B. A., S. M. Alaish, et al. (2007). "Testicular juvenile granulosa cell tumor in a newborn: case report<br />
and review <strong>of</strong> <strong>the</strong> literature." International Journal <strong>of</strong> Surgical <strong>Pathology</strong> 15(3): 321-325.<br />
Augusto, D., E. Leteurtre, et al. (2002). "Calretinin: a valuable marker <strong>of</strong> normal and neoplastic Leydig cells <strong>of</strong><br />
<strong>the</strong> testis." Applied Immunohistochemistry & Molecular Morphology 10(2): 159-162.<br />
Billings, S. D., L. M. Roth, et al. (1999). "Microcystic leydig cell tumors mimicking yolk sac tumor - A report<br />
<strong>of</strong> four cases." American Journal <strong>of</strong> Surgical <strong>Pathology</strong> 23(5): 546-551.<br />
Busam, K. J., K. Iversen, et al. (1998). "Immunoreactivity for A103, an antibody to Melan-A (MART-1), in<br />
adrenocortical and o<strong>the</strong>r steroid tumors." Am.J Surg.Pathol 22(1): 57-63.<br />
Carvajal-Carmona, L. G., N. A. Alam, et al. (2006). "Adult leydig cell tumors <strong>of</strong> <strong>the</strong> testis caused by germline<br />
fumarate hydratase mutations." J Clin Endocrinol Metab 91(8): 3071-3075.<br />
Cheville, J. C., T. J. Sebo, et al. (1998). "Leydig cell tumor <strong>of</strong> <strong>the</strong> testis - A clinicopathologic, DNA content,<br />
and MIB-1 comparison <strong>of</strong> nonmetastasizing and metastasizing tumors." American Journal <strong>of</strong> Surgical<br />
<strong>Pathology</strong> 22: 1361-1367.<br />
Comperat, E., F. Tissier, et al. (2004). "Non-Leydig sex-cord tumors <strong>of</strong> <strong>the</strong> testis. The place <strong>of</strong><br />
immunohistochemistry in diagnosis and prognosis. A study <strong>of</strong> twenty cases." Virchows Archiv: an International<br />
Journal <strong>of</strong> <strong>Pathology</strong> 444(6): 567-571.<br />
De Pinieux, G., C. Glaser, et al. (1999). "Testicular fibroma <strong>of</strong> gonadal stromal origin with minor sex cord<br />
elements - Clinicopathologic and immunohistochemical study <strong>of</strong> 2 cases." Archives <strong>of</strong> <strong>Pathology</strong> and<br />
Laboratory Medicine 123(5): 391-394.<br />
De Raeve, H., P. Schoonooghe, et al. (2003). "Malignant large cell calcifying Sertoli cell tumor <strong>of</strong> <strong>the</strong> testis."<br />
Pathol Res Pract 199(2): 113-117.<br />
Di Tonno, F., I. M. Tavolini, et al. (2009). "Lessons from 52 patients with leydig cell tumor <strong>of</strong> <strong>the</strong> testis: <strong>the</strong><br />
GUONE (North-Eastern Uro-Oncological Group, Italy) experience." Urol Int 82(2): 152-157.<br />
Drut, R., S. Wludarski, et al. (2006). "Leydig cell tumor <strong>of</strong> <strong>the</strong> testis with histological and<br />
immunohistochemical features <strong>of</strong> malignancy in a 1-year-old boy with isosexual pseudoprecocity."<br />
International Journal <strong>of</strong> Surgical <strong>Pathology</strong> 14(4): 344-348.<br />
Giannarini, G., A. Mogorovich, et al. (2007). "Long-term followup after elective testis sparing surgery for<br />
Leydig cell tumors: a single center experience." J Urol 178(3 Pt 1): 872-876; quiz 1129.<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 11
Hammerich, K. H., S. Hille, et al. (2008). "Malignant advanced granulosa cell tumor <strong>of</strong> <strong>the</strong> adult testis: case<br />
report and review <strong>of</strong> <strong>the</strong> literature." Human <strong>Pathology</strong> 39(5): 701-709.<br />
Harms, D. and L. R. Kock (1997). "Testicular juvenile granulosa cell and Sertoli cell tumours: A<br />
clinicopathological study <strong>of</strong> 29 cases from <strong>the</strong> Kiel Paediatric Tumour Registry." Virchows Archiv: an<br />
International Journal <strong>of</strong> <strong>Pathology</strong> 430(4): 301-309.<br />
Henley, J. D., R. H. Young, et al. (2002). "Malignant Sertoli cell tumors <strong>of</strong> <strong>the</strong> testis: a study <strong>of</strong> 13 examples <strong>of</strong><br />
a neoplasm frequently misinterpreted as seminoma." Am J Surg Pathol 26(5): 541-550.<br />
Iczkowski, K. A., D. G. Bostwick, et al. (1998). "Inhibin A is a sensitive and specific marker for testicular sex<br />
cord- stromal tumors." Modern <strong>Pathology</strong> 11(8): 774-779.<br />
Jimenez-Quintero, L. P., J. Y. Ro, et al. (1993). "Granulosa cell tumor <strong>of</strong> <strong>the</strong> adult testis: A clinicopathologic<br />
study <strong>of</strong> seven cases and a review <strong>of</strong> <strong>the</strong> literature." Human <strong>Pathology</strong> 24: 1120-1126.<br />
Jones, M. A., R. H. Young, et al. (1997). "Benign fibromatous tumors <strong>of</strong> <strong>the</strong> testis and paratesticular region: A<br />
report <strong>of</strong> 9 cases with a proposed classification <strong>of</strong> fibromatous tumors and tumor-like lesions." American<br />
Journal <strong>of</strong> Surgical <strong>Pathology</strong> 21(3): 296-305.<br />
Kato, N., M. Fukase, et al. (2001). "Sertoli-stromal cell tumor <strong>of</strong> <strong>the</strong> ovary: Immunohistochemical,<br />
ultrastructural, and genetic studies." Human <strong>Pathology</strong> 32(8): 796-802.<br />
Kim, I., R. H. Young, et al. (1985). "Leydig cell tumors <strong>of</strong> <strong>the</strong> testis. A clinicopathological analysis <strong>of</strong> 40 cases<br />
and review <strong>of</strong> <strong>the</strong> literature." American Journal <strong>of</strong> Surgical <strong>Pathology</strong> 9(3): 177-192.<br />
Kommoss, F., E. Oliva, et al. (2000). "Inhibin-alpha, CD99, HEA125, PLAP and chromogranin<br />
immunoreactivity in testicular neoplasms and <strong>the</strong> androgen insensitivity syndrome." Human <strong>Pathology</strong> 31(9):<br />
1055-1061.<br />
Kratzer, S. S., T. M. Ulbright, et al. (1997). "Large cell calcifying Sertoli cell tumor <strong>of</strong> <strong>the</strong> testis: contrasting<br />
features <strong>of</strong> six malignant and six benign tumors and a review <strong>of</strong> <strong>the</strong> literature." American Journal <strong>of</strong> Surgical<br />
<strong>Pathology</strong> 21(11): 1271-1280.<br />
Lawrence, W. D., R. H. Young, et al. (1985). "Juvenile granulosa cell tumor <strong>of</strong> <strong>the</strong> infantile testis. A report <strong>of</strong><br />
14 cases." Am J Surg Pathol 9(2): 87-94.<br />
Magro, G., A. Gurrera, et al. (2007). "Incompletely differentiated (unclassified) sex cord/gonadal stromal tumor<br />
<strong>of</strong> <strong>the</strong> testis with a "pure" spindle cell component: report <strong>of</strong> a case with diagnostic and histogenetic<br />
considerations." Pathol Res Pract 203(10): 759-762.<br />
McCluggage, W. G., J. H. Shanks, et al. (1998). "Immunohistochemical study <strong>of</strong> testicular sex cord stromal<br />
tumors, including staining with anti-inhibin antibody." American Journal <strong>of</strong> Surgical <strong>Pathology</strong> 22(5): 615-619.<br />
Nistal, M., R. L†zaro, et al. (1992). "Testicular granulosa cell tumor <strong>of</strong> <strong>the</strong> adult type." Archives <strong>of</strong> <strong>Pathology</strong><br />
and Laboratory Medicine 116: 284-287.<br />
Nistal, M., E. Redondo, et al. (1988). "Juvenile granulosa cell tumor <strong>of</strong> <strong>the</strong> testis." Arch Pathol Lab Med<br />
112(11): 1129-1132.<br />
Peterson, C. and S. Skoog (2008). "Prenatal diagnosis <strong>of</strong> juvenile granulosa cell tumor <strong>of</strong> <strong>the</strong> testis." J Pediatr<br />
Urol 4(6): 472-474.<br />
Petersson, F., S. Bulimbasic, et al. (2010). "Large cell calcifying Sertoli cell tumor: a clinicopathologic study <strong>of</strong><br />
1 malignant and 3 benign tumors using histomorphology, immunohistochemistry, ultrastructure, comparative<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 12
genomic hybridization, and polymerase chain reaction analysis <strong>of</strong> <strong>the</strong> PRKAR1A gene." Hum Pathol 41(4):<br />
552-559.<br />
Plata, C., F. Algaba, et al. (1995). "Large cell calcifying Sertoli cell tumour <strong>of</strong> <strong>the</strong> testis." Histopathology 26:<br />
255-259.<br />
Proppe, K. H. and R. E. Scully (1980). "Large-cell calcifying Sertoli cell tumor <strong>of</strong> <strong>the</strong> testis." Am J Clin Pathol<br />
74(5): 607-619.<br />
Renshaw, A. A., M. Gordon, et al. (1997). "Immunohistochemistry <strong>of</strong> unclassified sex cord-stromal tumors <strong>of</strong><br />
<strong>the</strong> testis with a predominance <strong>of</strong> spindle cells." Modern <strong>Pathology</strong> 10: 693-700.<br />
Rutgers, J. L., R. H. Young, et al. (1988). "The testicular "tumor" <strong>of</strong> <strong>the</strong> adrenogenital syndrome. A report <strong>of</strong> six<br />
cases and review <strong>of</strong> <strong>the</strong> literature on testicular masses in patients with adrenocortical disorders." Am J Surg<br />
Pathol 12(7): 503-513.<br />
Shukla, A. R., D. S. Huff, et al. (2004). "Juvenile granulosa cell tumor <strong>of</strong> <strong>the</strong> testis:: contemporary clinical<br />
management and pathological diagnosis." Journal <strong>of</strong> Urology 171(5): 1900-1902.<br />
Suardi, N., E. Strada, et al. (2009). "Leydig cell tumour <strong>of</strong> <strong>the</strong> testis: presentation, <strong>the</strong>rapy, long-term follow-up<br />
and <strong>the</strong> role <strong>of</strong> organ-sparing surgery in a single-institution experience." BJU Int 103(2): 197-200.<br />
Ulbright, T. M. (2008). "The most common, clinically significant misdiagnoses in testicular tumor pathology,<br />
and how to avoid <strong>the</strong>m." Advances in Anatomic <strong>Pathology</strong> 15(1): 18-27.<br />
Ulbright, T. M., M. B. Amin, et al. (2007). "Intratubular Large Cell Hyalinizing Sertoli Cell Neoplasia <strong>of</strong> <strong>the</strong><br />
<strong>Testis</strong>: A Report <strong>of</strong> 8 Cases <strong>of</strong> a Distinctive Lesion <strong>of</strong> <strong>the</strong> Peutz-Jeghers Syndrome." American Journal <strong>of</strong><br />
Surgical <strong>Pathology</strong> 31(6): 827-835.<br />
Ulbright, T. M., J. R. Srigley, et al. (2002). "Leydig cell tumors <strong>of</strong> <strong>the</strong> testis with unusual features - Adipose<br />
differentiation, calcification with ossification, and spindle-shaped tumor cells." American Journal <strong>of</strong> Surgical<br />
<strong>Pathology</strong> 26(11): 1424-1433.<br />
Ulbright, T. M., J. R. Srigley, et al. (2002). "Leydig cell tumors <strong>of</strong> <strong>the</strong> testis with unusual features: adipose<br />
differentiation, calcification with ossification, and spindle-shaped tumor cells." Am J Surg Pathol 26(11): 1424-<br />
1433.<br />
Venara, M., R. Rey, et al. (2001). "Sertoli cell proliferations <strong>of</strong> <strong>the</strong> infantile testis - An intratubular form <strong>of</strong><br />
Sertoli cell tumor?" American Journal <strong>of</strong> Surgical <strong>Pathology</strong> 25(10): 1237-1244.<br />
Young, R. H., D. D. Koelliker, et al. (1998). "Sertoli cell tumors <strong>of</strong> <strong>the</strong> testis, not o<strong>the</strong>r-wise specified - A<br />
clinicopathologic analysis <strong>of</strong> 60 cases." American Journal <strong>of</strong> Surgical <strong>Pathology</strong> 22(6): 709-721.<br />
Young, S., S. Gooneratne, et al. (1995). "Feminizing Sertoli cell tumors in boys with Peutz-Jeghers syndrome."<br />
American Journal <strong>of</strong> Surgical <strong>Pathology</strong> 19: 50-58.<br />
Zukerberg, L. R., R. H. Young, et al. (1991). "Sclerosing Sertoli cell tumor <strong>of</strong> <strong>the</strong> testis. A report <strong>of</strong> 10 cases."<br />
American Journal <strong>of</strong> Surgical <strong>Pathology</strong> 15(9): 829-834.<br />
Zaloudek <strong>Testis</strong> <strong>Sex</strong> <strong>Cord</strong>‐<strong>Stromal</strong> <strong>Tumors</strong> Page 13