What are Staphylococcal infections?
Staphylococcal infections are caused by the bacterium Staphylococcus. Infection symptoms range in severity, from skin conditions like boils to blood infections like sepsis.
- Staphylococcal infections are caused by the bacterium Staphylococcus. The most common bacterium in this group is Staphylococcus aureus.
- They are spread by skin-to-skin contact, often starting by infecting small cuts in the skin.
- There’s a wide spectrum of Staphylococcal infections, both in terms of severity and how easily they can be treated.
What are the symptoms of Staphylococcal infections?
Staphylococcal infections occur when the bacterium gets into the body through a break or cut in the skin. Depending on how far they get into the body, the infections are usually divided into two groups:
- skin and soft tissue infections – which tend to be less severe
- invasive infections – which can create considerable damage to organs and tissues
Skin and soft tissue Staphylococcal infections include:
- Boils:painful, red bumps on the skin of the neck, face, thighs, armpits and buttocks
- Impetigo: a highly contagious skin infection causing painful sores and painless blisters
- Cellulitis: an infection of the deepest layer of the skin and the layer of fat and soft tissue beneath the skin. This can cause patients to feel feverish and nauseous.
Invasive Staphylococcal infections include:
- Sepsis, or blood poisoning: the Staphylococcus bacteria have entered the blood stream, triggering an overwhelming immune response. This is a medical emergency.
- Symptoms include fever, fast heartbeat, low blood pressure, diarrhoea, pale and cold skin, and sometimes loss of consciousness.
- Toxic shock syndrome is a rare but life-threatening form of severe sepsis, caused when the bacteria release a toxic substance. It causes a high fever, a dramatic drop in blood pressure (shock), dizziness and confusion.
- Septic arthritis: the Staphylococcus bacteria have infected the joints, causing swelling, pain and fever.
- Endocarditis: the Staphylococcus bacteria have infected the internal structures of the heart, such as the heart valves, causing inflammation.
- Symptoms include chest pain, coughs, fatigue, shortness of breath, fever and unexplained weight loss. They can develop gradually over many weeks, or quickly over a few days.

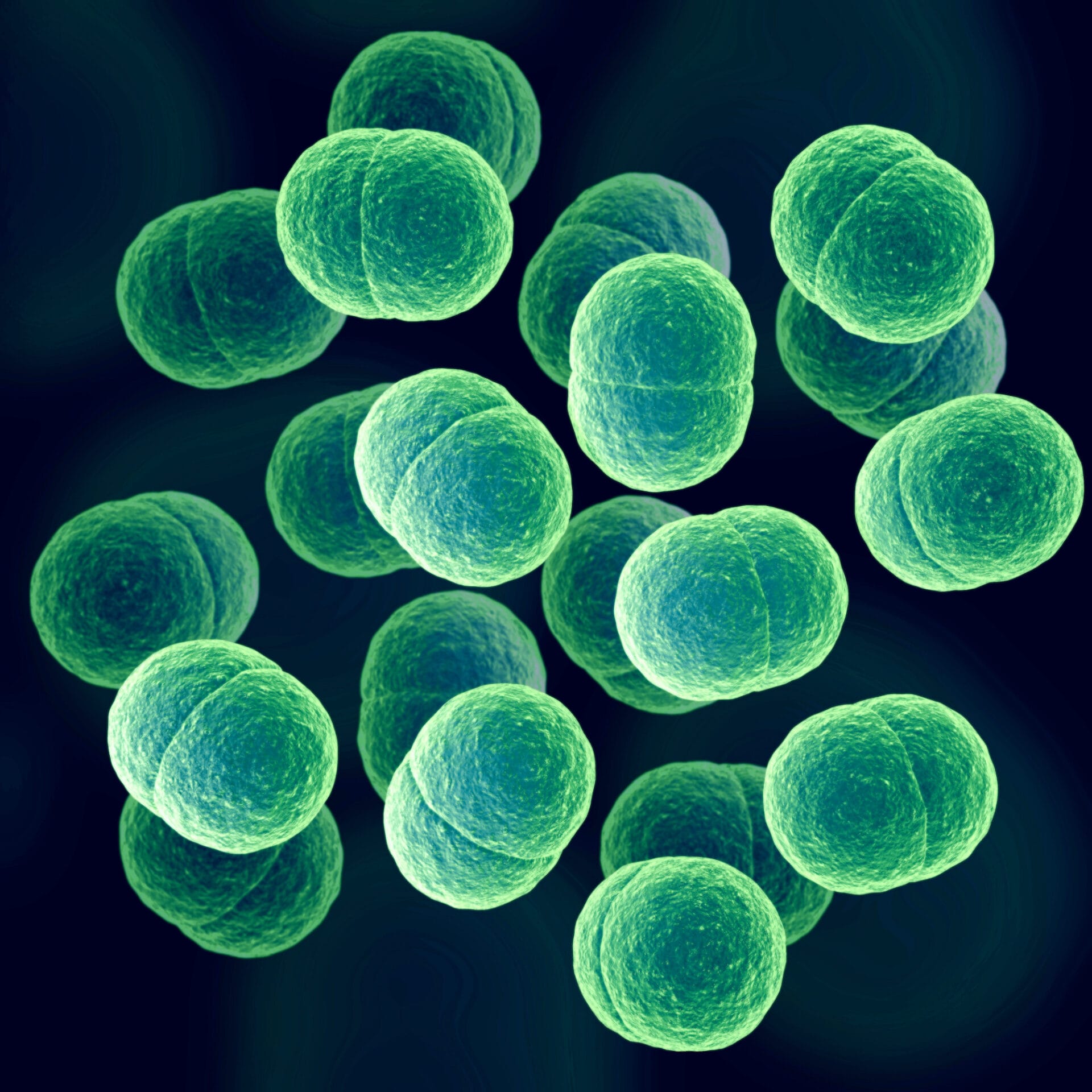
A plate of Staphylococcus aureus. Image credit: Valugi / via Wikimedia Commons
Treating Staphylococcal infections
- The doctor will assess the type, site and severity of the infection to identify the best course of treatment.
- Skin and soft tissue infections are usually milder and can be treated with antibiotic tablets or creams. Boils may be treated with a technique called ‘incision and drainage’, to drain pus and relieve pressure and pain.
- For more invasive infections, doctors may have to deliver antibiotics by injection or drip. These may be given for up to several months, depending on how serious the infection is.
- However, many strains of Staphylococcal bacteria have become resistant to antibiotics. This includes MRSA (Methicillin-resistant Staphylococcus aureus), which is resistant to several antibiotics, including methicillin.
- To treat MRSA, the doctor will investigate which antibiotics the strain is resistant or sensitive to. Some strains can still be treated effectively with other antibiotics, or a combination of antibiotics.
What is methicillin-resistant Staphylococcus aureus (MRSA)?
- MRSA is a strain of Staphylococcal infection that many of us live with in our nose or skin, without knowing or having any symptoms. This is called being a ‘silent carrier’ of the bacterium.
- A small proportion of people develop an infection, if the bacteria enters the body through an area of broken skin, such as a wound.
- MRSA is sometimes referred to as a ‘superbug’. It causes more problems than regular Staphylococcus aureus because it is resistant to many common antibiotics. This makes it difficult to treat, and quick to spread.
- MRSA often spreads quickly in hospitals and care homes, putting a huge strain on healthcare systems. Since many people in these settings are older or weaker, they may be more vulnerable to a life-threatening infection.
Preventing the spread of MRSA
Increased awareness of MRSA in recent years has helped healthcare professionals to manage it more effectively. Prevention techniques include:
- washing hands before and after visiting someone in a care home or hospital
- screening patients for MRSA before they are admitted to hospital for an operation
- putting all disposable items, such as dressings and gloves, into the appropriate bins promptly to avoid cross-contamination
- encouraging patients and families to speak to their nurse or doctor if they are worried about hygiene standards on a ward.