Endometriosis assessment
What Is Endometriosis?
Definition
Endometriosis is defined as the presence of normal tissue of the lining of the uterus (endometrium) in an abnormal place, usually the female pelvis. The most common sites in the pelvis are on and below the ovaries, and deep in the pelvis behind the uterus, called the Pouch of Douglas. Here the endometriosis grows on the ligaments behind the uterus and on the vagina and rectum. It also may grow on the bladder, appendix, and even sometimes in the upper abdomen or in the abdominal wall in scars of a laparoscopy or caesarean section.
Symptoms
Pain during periods
Pain with sexual intercourse
Pain on defecation with periods
Chronic pelvic pain
Abnormal bleeding
Pain when urinating
Infertility
Pain with ovulation
Fatigue
To make it confusing, some people with endometriosis have severe symptoms and others have very mild to sometimes hardly any symptoms. On the other hand, women who have the symptoms of endometriosis do not always have the disease.
Why does it occur?
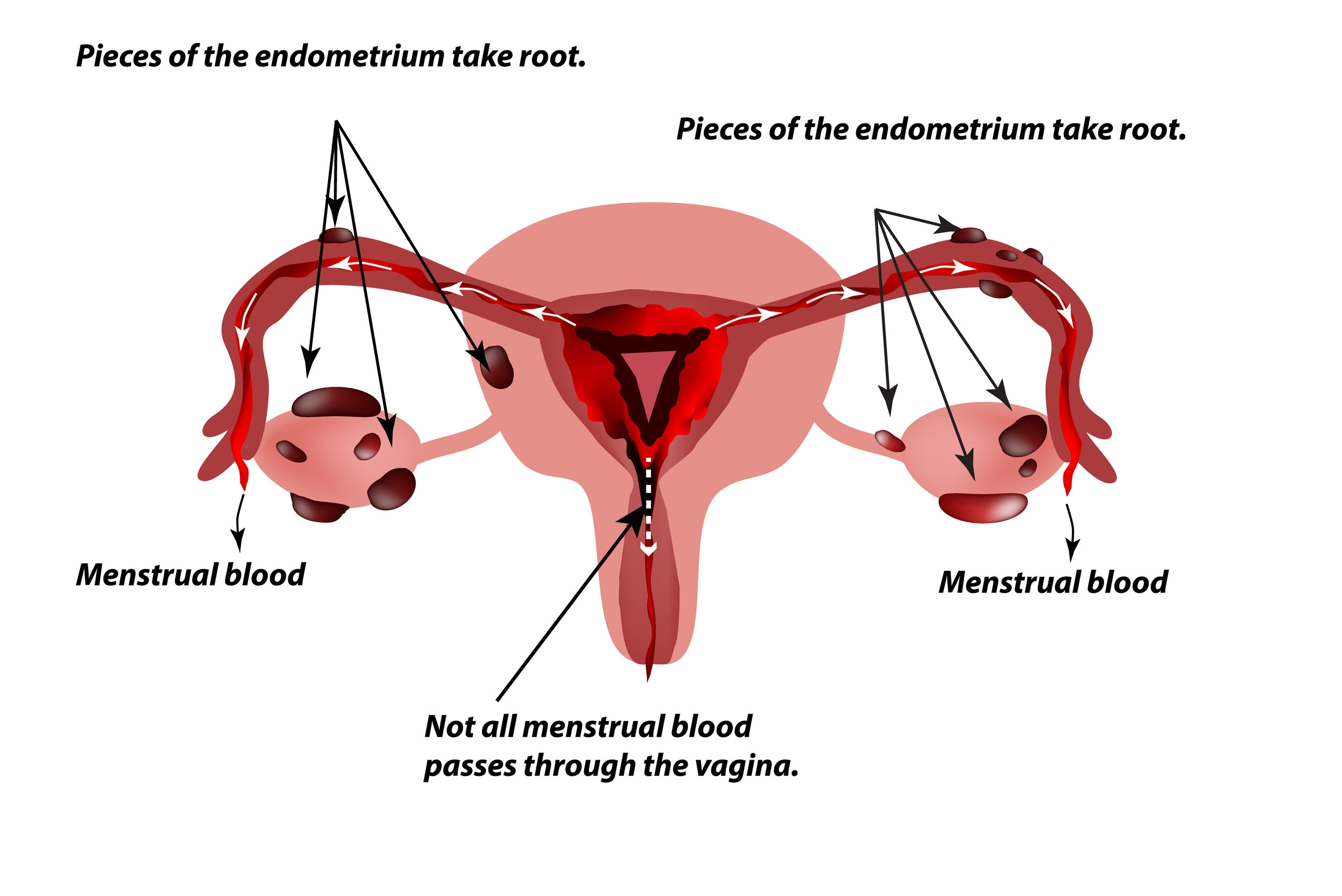
The main mechanism believed responsible is backwards flow of menstrual blood through the Fallopian tubes into the pelvis during periods. The cells of the lining of the uterus (endometrial cells) can then implant in the pelvis and give rise to endometriosis lesions.
Different Forms
A distinction is made between superficial lesions and deep infiltrating endometriosis.
In the majority of women with endometriosis the lining of the uterus found in the pelvis has only implanted superficially. These lesions may present as raised black or brown lesions, white discolouration, red "flame-like" streaks, clear blisters, small red blisters, bluish lesions or yellow patches.
About 20% of women however will not just allow the lining cells to implant in the pelvis, but also to infiltrate mainly into bowel, bladder, the vagina and ligaments behind the uterus (uterosacral ligaments). This form of the disease is called deep infiltrating endometriosis (DIE). Deep infiltrating endometriosis causes usually more destruction of the normal anatomy and is generally significantly more difficult to treat. Because lesions of endometriosis infiltrate into ligaments, vagina, bowel and bladder, adhesions can occur between organs such as the bowel and the uterus or the uterus and the ovaries.
What Can the Ultrasound diagnose?
Superficial lesions of endometriosis can never be diagnosed on ultrasound as these lesions have no real mass, only colour, which can not be detected with ultrasound. The lesions look like brown small 'blood splatters' which are implanted on variousareas in the pelvis. These lesions can only be seen on laparoscopy. They are generally easy to remove. Special preoperative measures are rarely required. They can however cause as much or more pain than some deep infiltrating lesions.
Deep infiltrating endometriosis causes usually more destruction of the normal anatomy. Because lesions of endometriosis infiltrate into ligaments, bowel and bladder, a little 'clump' or 'nodule' is formed, which does have mass and can be detected with ultrasound. Also the adhesions that can occur between organs such as the bowel and the uterus or the uterus and the ovaries can be seen with ultrasound.
Often when deep infiltrating endometriosis is unexpectedly found at laparoscopy, without a preoperative diagnosis with ultrasound, the removal of endometriosis can not be completed as special preparation is required to allow removal of such lesions. The patient needs to take bowel preparation to allow surgery on the bowel, and often it is preferable to have a colorectal surgeon present at the surgery. If these lesions are diagnosed preoperatively, the necessary preparations can be made prior to starting the first laparoscopy andrepeat surgery can be avoided.
The larger the lesion, the easier it is to see on ultrasound, but in the hands of experienced imaging specialists lesions of only a few millimetres can be diagnosed.
In summary, an ultrasound can never completely rule out endometriosis because the superficial type of endometriosis can not be diagnosed with ultrasound. A laparoscopy may still be required to rule out endometriosis if symptoms are significant. But if the ultrasound was normal, there is a good chance that even if endometriosis is found at laparoscopy, it will be possible to complete the removal of most lesions. DIE on the other hand can rarely be removed at first surgery, unless its presence was known preoperatively. Because ultrasound can diagnose these lesions, the surgery can be planned better and repeat surgery is less commonly necessary.
How is the ultrasound performed?
Because endometriosis mainly occurs behind the uterus, an area that can not be seen well on transabdominal ultrasound, a vaginal ultrasound will allow much better views. A narrow, gel covered probe is gently introduced into the vagina. You will be asked to empty your bladder before the scan for your comfort as well as to optimise our views. The examination takes approximately 20 minutes.
If your doctor refers you specifically to look for endometriosis and you feel uncomfortable about having a vaginal ultrasound or if you have never had sexual intercourse, in which case a vaginal scan is not advisable, please advise our receptionist and she will discuss it with the doctor as an MRI may be a better way to look for deep infiltrating endometriosis in your situation.
A normal transvaginal ultrasound will be performed. Some patients are told that the scan is done transrectally but this is not the case.
The ultrasound usually takes 30 minutes. The result are often discussed with you and will be sent to your referring doctor.
Because endometriosis can infiltrate the bowel, the doctor or sonographer who does the ultrasound will carefully look at the bowel during the transvaginal ultrasound. When the rectum is empty, the views of the bowel are generally better as bowel content can cause shadows on ultrasound. A mild bowel preparation prior to the ultrasound may optimise the views when you have had a past history of severe endometriosis or when you have significant bowel pain during your periods. This consists of a mild laxative the night before the ultrasound and an enema within an hour before the ultrasound as outlined below. If you don't have a proven history of significant endometriosis, or no significant bowel symptoms, it is probably not necessary to take bowel preparation.
Bowel preparation
The bowel preparation is always mild and usually well tolerated and is outlined below. All the medication is over the counter medication. It is cheap and does not require a script. Make sure the chemist gives the fleet enema rather than the oral fleet.
The night before the scan take
Dulcolax tablet, one tablet of 5mg or Dulcolax SP 10 drop
This is mild laxative that will make it easy to go to the toilet the next morning. Some people experience some cramping.
Just before the scan
Fleet enema
A fleet enema is a bottle with 133ml of liquid in it. It has a nozzle that is precovered with gel. Apply it while lying on your side, inserting the nozzle into the anus and squirting the full content of the bottle into the rectum. An urge to go to the toilet will follow application. Try to wait 3 to 5 minutes before going to the toilet. After this your rectum should be completely empty optimising ultrasound images.