Published online Oct 16, 2023. doi: 10.12998/wjcc.v11.i29.7107
Peer-review started: June 6, 2023
First decision: August 30, 2023
Revised: September 8, 2023
Accepted: September 22, 2023
Article in press: September 22, 2023
Published online: October 16, 2023
Giant condyloma acuminatum (GCA) is an uncommon condition affecting the anogenital area.
Here, we report an 88-year-old male patient who presented with a 5-year history of a progressive appearance of multiple cauliflower-like warts over his penile shaft, pubis region, and groin as well as urine leakage along the distal penile shaft. Physical examination revealed an ulcerative skin perforation with pus discharge under the distal prepuce base, which was initially suspected to be a urethral fistula. However, during surgery, it was discovered that the perforation was caused by a giant condyloma lesion that had obliterated the prepuce opening, with infection and high pressure causing subsequent skin perforation. He underwent circumcision and wide excision with electrocauterization of the warts. He was discharged after the surgery, and the residual lesion was treated with imiquimod and low-dose oral tegafur-uracil.
Penile GCA can cause prepuce perforation and can be postoperatively treated with imiquimod and low-dose oral tegafur-uracil.
Core Tip: This case report highlights a rare presentation of a giant condyloma acuminatum (GCA) in an elderly male patient. The patient presented with progressive, cauliflower-like warts on the penile shaft, pubis region, and groin, accompanied by urine leakage and an ulcerative skin perforation with pus discharge under the prepuce. Surgery revealed that the perforation was caused by an obliterative giant condyloma lesion, mimicking urethral rupture. The patient underwent circumcision, wide excision of warts, and tailored subsequent treatment with favorable outcomes. This case emphasizes the importance of individualized treatment for GCA and the successful management of spontaneous prepuce perforation.
- Citation: Hsu FC, Yu DS, Pu TW, Wu MJ, Meng E. Unusual presentation of penile giant condyloma acuminatum with spontaneous prepuce perforation: A case report. World J Clin Cases 2023; 11(29): 7107-7112
- URL: https://www.wjgnet.com/2307-8960/full/v11/i29/7107.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i29.7107
Giant condyloma acuminatum (GCA), also known as Buschke-Lowenstein tumor, was first reported by Abraham Buschke in 1896 and later by Loewenstein in 1925[1]. It typically appears as a slowly growing mass resembling a cauliflower in the genital or anorectal region. The tumor tends to infiltrate deeper tissues at a relatively slow rate[2]. Here, we present a case of penile GCA where the initial symptom mimicked a urethral fistula resulting from the obliteration of the preputial opening by the giant condyloma lesion and subsequent perforation of the distal preputial skin.
An 88-year-old male patient complained of multiple warts over the pubis region and exogenitalia for 5 years and urine leakage from the distal penis noted for 2 wk.
He denied multiple sexual partners. The patient was not immunocompromised and was negative for human immunodeficiency virus and syphilis.
The patient denied any prior systemic diseases.
The family history revealed nothing noteworthy.
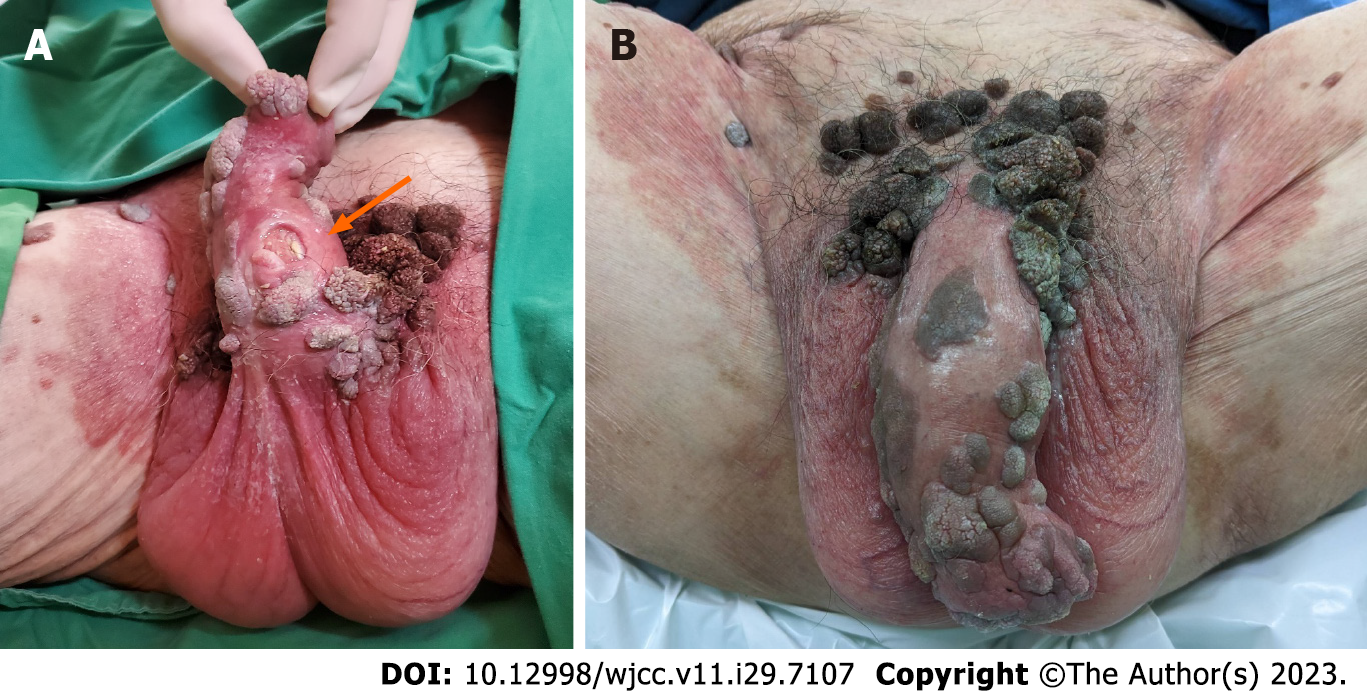
Physical examination revealed an ulcerative distal preputial hole, measuring 1 cm in diameter, with pus discharge under the ventral penile shaft so that the initial impression was a urethral fistula (Figure 1A). In addition, multiple condyloma lesions and plaques, presenting as cauliflower-like warts, were noted over the exogenitalia, penile shaft, pubis, and groin region (Figure 1B). The warts were clustered, gray-to-black in color, hard, and not painful. Some warts were spread sporadically over the scrotum, and multiple verrucous plaques were also found in the perianal region on rectal examination.
A serum test revealed leukocytosis with elevated white blood cell levels of 12.13 (103/μL). The urine sediment examination revealed pyuria, characterized by an elevated urine white blood cell count of 10-20 per high-power field. All lab results were found to be normal during the follow-up interval.
Distant metastasis was excluded through chest and abdominal computed tomography scans.
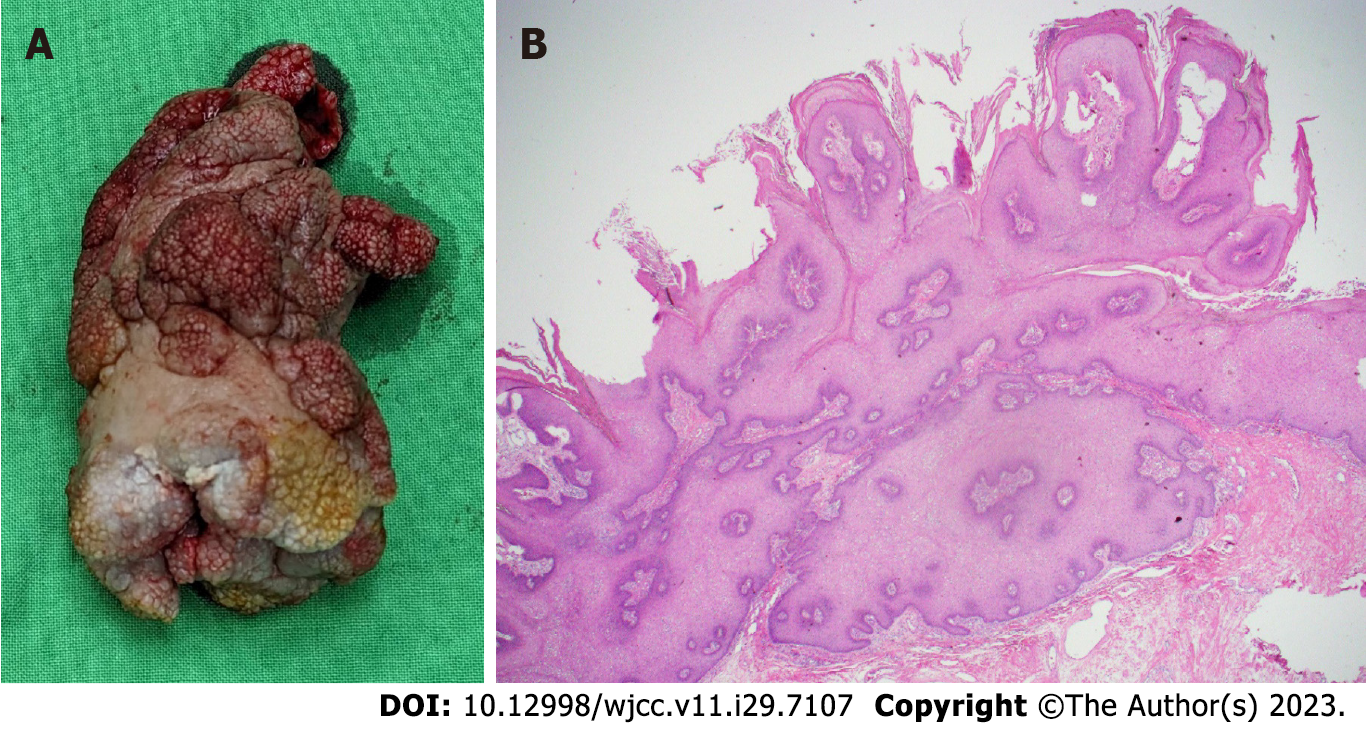
The pathology of the circumcised redundant prepuce (Figure 2) confirmed the diagnosis of giant condyloma acuminata with moderate dysplasia and destructive local invasion without metastasizing. The human papillomavirus (HPV) genotyping results for the redundant prepuce specimen indicated a positive presence of HPV-11.
During the operation, we found that the prepuce opening was completely obliterated by a giant condyloma lesion with a distal preputial perforation, which mimicked a urethral fistula. Urine drained from a spontaneous perforation that was present directly below the glans, nearly at the level of the coronal sulcus. Finally, circumcision along the hole and wide excision with electrocauterization of the residual warts were performed.
The postoperative course was uneventful, and the wounds healed gradually with adjuvant topical 5% imiquimod cream thrice a week and oral tegafur-uracil (UFUR), containing 100 mg of tegafur and 224 mg of uracil, two pills per day, for 6 mo (Figure 3).
CA lesions, which grow extensively and display invasive local growth patterns without spreading to distant sites, are referred to as Buschke-Löwenstein tumors. These tumors are also known as verrucous carcinoma or giant condylomas. Buschke-Lowenstein tumors were first reported by Abraham Buschke in 1896 and later by Loewenstein in 1925[1]. GCA is an uncommon condition that is characterized by a cauliflower-like growth with exophytic extension and tends to invade nearby tissues. This condition has a high rate of recurrence and carries the potential for malignant transformation[3]. GCA is associated with various types of HPV, immunosuppression, and other risk factors that require further investigation. GCA is associated with several factors, such as having multiple sexual partners, chronic genital infections, poor hygiene, and immunodeficiencies[4].
An estimated prevalence of 0.1% has been reported in the general population, with the condition usually presenting between the 4th and 6th decades of life[3,5]. In the latest case series, the male-to-female ratio was reported as 2.7:1, with patients ranging in age from 24 to 77 years old and a mean age of 43.9 years. Additionally, there was a tendency for the condition to present at younger ages[6].
Cases of GCA have been reported in the pediatric age group, and a limited number of cases also have been reported in pregnant women[7,8]. The types of HPV causing condyloma acuminatum warts of the anal and genital regions were 6, 11, 42, 44, and 54[9]. Persistent HPV infection was observed in 10% of patients with GCA, and the progression to invasive cancer in such cases typically extends over a 15 to 20-year timeframe[10]. Intraepithelial neoplasia commonly arises during the subclinical phase, while the clinical phase is characterized by the presence of visible lesions and symptoms such as condyloma acuminatum or invasive cancer[11]. Papillomatous lesions are frequently observed in the male genital area, including the penis, scrotum, urethral opening, and perianal region, and in the female genital area, including the vaginal opening, vulva, perineum, and perianal region.
Because of the absence of a dependable serological test to distinguish between past and current HPV infections and the inability to isolate the virus, the definitive diagnosis relies on the detection of HPV-DNA using molecular tests. Nucleic acid amplification tests, such as polymerase chain reaction (PCR), are presently employed as the established benchmark for HPV genotyping[12]. At present, there is no universally agreed-upon standard for the most effective sampling technique for HPV DNA genotyping among circumcised heterosexual men. Sarier et al[13] designed a study involving six different anatomical sampling sites for HPV DNA PCR testing in circumcised heterosexual men with genital warts. Their findings revealed that the detection rate approaches 99% when wart biopsy is combined with swab sampling of the penile shaft, coronal sulcus, scrotum, and external urethral meatus[13].
GCA is primarily characterized by the presence of a perineal mass, but patients may also experience symptoms such as constipation, hemorrhoids, difficulty defecating and urinating, dysuria, abdominal distension, and fatigue[2]. Interestingly, based on initial examination, our case presented as a urethral fistula resulting from an obstruction in the urethra, caused by the growth of GCA up to the meatus. It was not until further surgical examination that we discovered that the preputial opening had been obstructed by GCA, causing the perforated prepuce to present in a manner mimicking a urethral fistula. This event has not been reported in GCA-related case studies. Theoretically, the slow growth pattern of GCA led to chronic inflammation and infection within the prepuce, resulting in the accumulation of pus and eventual spontaneous perforation of the prepuce. The resulting perforated hole allowed for urine diversion and successful decompression of preputial obstruction.
The malignancy of GCA can be considered in two distinct ways: Through the confirmation of neoplastic histology in malignant transformation and through the infiltration of adjacent deep tissues, regardless of whether histological confirmation of malignancy is present, in the case of malignant behavior. Trombetta and Place[6] reported that in their series of 51 patients with GCA, 58% of the patients had neoplasia present at the time of diagnosis. Chu et al[2] observed a neoplastic transformation rate of 56% in their series of 42 patients with GCA, as 56% of the patients had histologically confirmed malignancy during follow-up. In cases where squamous cell carcinoma develops in the presence of GCA, treatment must be tailored to the patient’s individual circumstances, and in some cases, only palliative care may be provided to prevent the development of further comorbidities[14].
In the past, various therapeutic options have been used for the treatment of GCA, including topical chemotherapy, intralesional injection of 5-fluoracil (5-FU), interferon, cryotherapy, curettage, CO2 Laser vaporization, wide resection alone or with neoadjuvant or adjuvant chemotherapy, chemotherapy alone, radiation therapy, and isolated perfusion[2]. Nevertheless, a universally accepted treatment approach with optimal effectiveness for anogenital warts remains elusive. It is understood that even after the disappearance of visible lesions following treatment, the virus can still be detected in apparently normal epithelial tissue for several months. The use of podophyllin, which inhibits cell division during the metaphase stage and induces localized tissue necrosis, resulting in the eradication of warts, has yielded unsatisfactory outcomes for GCA, but it has demonstrated positive outcomes for cases of classic condyloma acuminatum[2]. In the highly uncommon instances of extragenital GCA where resection is restricted owing to potential functional impairment, the use of combined therapy involving topical podophyllotoxin and imiquimod, along with weekly cryotherapy, has been documented as effective. This approach offers advantages over surgical treatment alone, as it does not result in functional consequences[15]. Surgical excision is particularly favored for solitary and giant genital verrucous lesions because it allows for both therapeutic intervention and diagnostic pathological assessment to detect precancerous changes[11]. Performing surgical treatment with negative margins is currently considered the optimal approach and should be pursued whenever feasible[16]. In the field of urology, surgical excision is particularly effective when dealing with cases of anterior urethral carcinoma[17]. Various treatment combinations, in addition to surgery as both neoadjuvant and adjuvant therapy, have been reported, yielding varying outcomes[18]. However, there is no standardized selection process to determine the appropriate therapeutic approach. It is advisable to adopt an individualized therapeutic approach for each case[19]. There are multiple options for surgical treatment to remove GCA, including traditional surgery, as well as alternative methods such as electrocoagulation, radiofrequency, and carbon laser surgery, which is used for intraurethral and common extragenital verrucas. Because of the high likelihood of recurrence, it is strongly advised to conduct long-term follow-up for individuals with GCA[20].
Although the estimated rate of malignant transformation is as high as 56%, there is no propensity for metastasis[2]. In addition, given the advanced age of the patient and the recommended first-line treatment protocol of 5-FU-based chemotherapy[6], we tailored a treatment plan for this patient that involved local wide excision with circumcision and electrocautery combined with adjuvant topical 5% imiquimod cream thrice a week and oral UFUR, containing 100 mg of tegafur and 224 mg of uracil, two pills per day, rather than a more aggressive reconstructive surgery. The patient continued to use the above medication for six months, and the wound remained in good condition without new local wart recurrence.
While it is rare to see penile GCA cases mimicking a urethral fistula, our case demonstrates that obliteration of the preputial opening in GCA can cause spontaneous prepuce perforation. The obliteration of the prepuce and glans by GCA caused chronic inflammation and infection, with eventual spontaneous perforation of the prepuce.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ali N, Finland; Sarier M, Turkey S-Editor: Wang JJ L-Editor: A P-Editor: Yuan YY
| 1. | Steffen C. The men behind the eponym--Abraham Buschke and Ludwig Lowenstein: giant condyloma (Buschke-Loewenstein). Am J Dermatopathol. 2006;28:526-536. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Chu QD, Vezeridis MP, Libbey NP, Wanebo HJ. Giant condyloma acuminatum (Buschke-Lowenstein tumor) of the anorectal and perianal regions. Analysis of 42 cases. Dis Colon Rectum. 1994;37:950-957. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Ben Kridis W, Werda I, Charfi S, Toumi N, Boudawara T, Mzali R, Daoud J, Khanfir A. Buschke - Lowenstein anal tumor: an ambiguous entity. Exp Oncol. 2019;41:182-184. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Bazouti S, Zizi N, Dikhaye S. Perianal giant condyloma Acuminatum-Buschke-Löwenstein tumor. Presse Med. 2019;48:584-585. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | El Bessi M, Dougaz W, Jones M, Jerraya H, Dziri C. A Giant Anorectal Condyloma Is Not Synonym of Malignancy. J Gastrointest Cancer. 2019;50:1026-1028. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Trombetta LJ, Place RJ. Giant condyloma acuminatum of the anorectum: trends in epidemiology and management: report of a case and review of the literature. Dis Colon Rectum. 2001;44:1878-1886. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Sikanić Dugić N, Ljubojević Hadžavdić S, Pustišek N, Hiršl Hećej V. Treatment of anogenital warts in an 18-month-old girl with 5% imiquimod cream. Acta Dermatovenerol Croat. 2014;22:40-43. [PubMed] [Cited in This Article: ] |
| 8. | Cui T, Huang J, Lv B, Yao Q. Giant condyloma acuminatum in pregnancy: A case report. Dermatol Ther. 2019;32:e12972. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Burk RD, Ho GY, Beardsley L, Lempa M, Peters M, Bierman R. Sexual behavior and partner characteristics are the predominant risk factors for genital human papillomavirus infection in young women. J Infect Dis. 1996;174:679-689. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV, Snijders PJ, Meijer CJ; International Agency for Research on Cancer Multicenter Cervical Cancer Study Group. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518-527. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Scheinfeld N. Update on the treatment of genital warts. Dermatol Online J. 2013;19:18559. [PubMed] [Cited in This Article: ] |
| 12. | Abreu AL, Souza RP, Gimenes F, Consolaro ME. A review of methods for detect human Papillomavirus infection. Virol J. 2012;9:262. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | Sarier M, Sepin N, Emek M, Konuk EY, Kaplan T, Yuksel BA, Barut Z, Cakcak DS, Hoscan MB. Evaluation of the optimal sampling approach for HPV genotyping in circumcised heterosexual men with genital warts. J Infect Chemother. 2023;29:475-480. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Papapanagiotou IK, Migklis K, Ioannidou G, Xesfyngi D, Kalles V, Mariolis-Sapsakos T, Terzakis E. Giant condyloma acuminatum-malignant transformation. Clin Case Rep. 2017;5:537-538. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Lee CN, Hsu CK, Lee JY. Recalcitrant extragenital giant condyloma acuminatum: A need for combination therapy. Dermatol Ther. 2019;32:e12867. [PubMed] [DOI] [Cited in This Article: ] |
| 16. | Badiu DC, Manea CA, Mandu M, Chiperi V, Marin IE, Mehedintu C, Popa CC, David OI, Bratila E, Grigorean VT. Giant Perineal Condyloma Acuminatum (Buschke-Lowenstein Tumour): A Case Report. Chirurgia (Bucur). 2016;111:435-438. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | Yilmaz Ö, Okçelik S, Soydan H, Ateş F, Yeşildal C, Aktaş Z, Şenkul T. Our urethrocutaneous fistula repair results in adults after hypospadias surgery. Rev Int Androl. 2018;16:143-146. [PubMed] [DOI] [Cited in This Article: ] |
| 18. | Jorgaqi E, Jafferany M. Giant condyloma acuminatum (Buschke-Lowenstein tumor): Combined treatment with surgery and chemotherapy. Dermatol Ther. 2020;33:e13193. [PubMed] [DOI] [Cited in This Article: ] |
| 19. | Diaz Gómez CJ. "Giant Condyloma Acuminatum (Buschke-Lowenstein tumor): Combined treatment with surgery and chemotherapy."-Further points to be discussed. Dermatol Ther. 2020;33:e13268. [PubMed] [DOI] [Cited in This Article: ] |
| 20. | Spinu D, Rădulescu A, Bratu O, Checheriţă IA, Ranetti AE, Mischianu D; -. Giant condyloma acuminatum - Buschke-Lowenstein disease - a literature review. Chirurgia (Bucur). 2014;109:445-450. [PubMed] [Cited in This Article: ] |