A very small percentage of women have a heart-shaped uterus (womb). This condition is known as a bicornuate uterus, and it can sometimes affect your fertility and pregnancy. This is called a congenital uterine abnormality. It means that your uterus formed in an unusual way before you were born, and has two sections divided by a septum or wall of tissue. Around 3.9% of women are born with a defect of the uterus.
Most women are unaware that they have an abnormality as there often aren’t any symptoms, and may only find out during an ultrasound scan or if they have experienced miscarriage, bleeding or difficulty conceiving. Although these abnormalities are quite common, the effect they have on a pregnancy isn’t always certain and won’t necessarily affect the ability to conceive.
The shape of the uterine cavity can affect how a baby lies during pregnancy and may be more difficult to carry a baby to full-term. Depending on the type of bicornuate uterus, there may be an increased risk of miscarriage or preterm delivery (giving birth before 37 weeks). Some studies have shown that these problems happen because of reduced capacity within the uterus and irregular uterine contractions. A uterine abnormality can also be linked to a weaker cervix (sometimes called cervical incompetence), which can lead to preterm birth. You may need extra monitoring during pregnancy, and Consultant – led care to keep you and your baby safe.
A bicornuate uterus is characterised by a cleft on the upper fundus, which gives it a heart shape. The uterus is malformed during organogenesis, part of embryonic development of the female fetus in her mother’s womb. A normal uterus is formed in a female fetus during the 5th week of pregnancy. The formation begins when two unrelated horn-like structures called Müllerian ducts move down into the pelvis and fuse together, forming the uterus. The septum indicates the zone of fusion and isolates the two structures. This is later reabsorbed to make an intrauterine cavity. A bicornuate uterus is formed when the Müllerian ducts move into the pelvis, but do not fuse completely. The upper portion dips inward while the lower portion remains normal. This partial non-fusion of the Müllerian ducts at the level of the uterine fundus is characterized by the presence of a cleft > 1 cm in the external contour of the top of the uterus. There are varying degrees of non-fusion giving rise to different types of uterine shape which are characterised into groups.
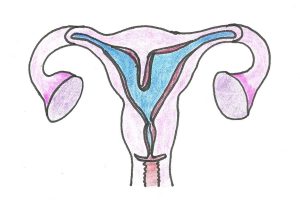
Outlined below are the different types of uterine abnormality, and a brief description of the affect it might have on pregnancy. The first drawing of a female reproductive system shows a normal uterus.
Normal uterus: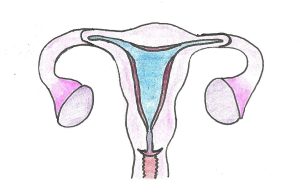
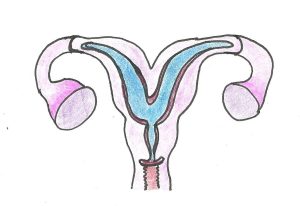
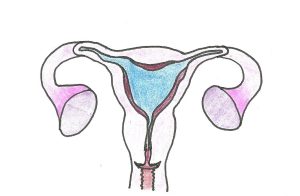
Bicornuate uterus:
A bicornuate uterus has a deep indentation at the top. Women with a bicornuate uterus have no extra difficulties with conception or in early pregnancy, but studies have shown that there is a slightly higher risk of miscarriage and preterm birth. It can also affect the baby’s position later in the pregnancy, and if the baby is breech, a Caesarean section might be recommended.
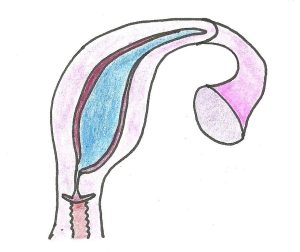
Unicornuate uterus:
Having a unicornuate womb is rare. It means your uterus is half the size of a normal womb because one side didn’t develop. There is an increased risk of ectopic pregnancy (an abnormal pregnancy that implants and develops outside the womb), late miscarriage or preterm birth. The baby may lie in an awkward position in later pregnancy so a Caesarean section might be required. Women who have a unicornuate uterus can conceive, although studies have shown that this type of rare anomaly is more common in women who are infertile.
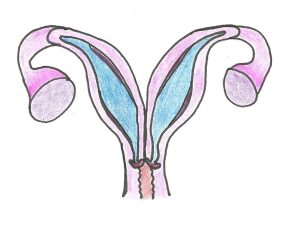
Didelphic (double) uterus:
The didelphic uterus is split in two, with each side having its own cavity. This usually affects the womb and cervix, but it can also affect the vulva, bladder, urethra and vagina. Women with a didelphic uterus have no extra difficulties with conception and studies have linked it to a small increase in the risk of preterm birth.
Septate/subseptate womb
A septate womb has a wall of muscle coming down the centre splitting the uterine cavity into two spaces. A septate uterus will have a band of muscle tissue extending through the whole uterine cavity, whereas in a subseptate uterus it may only extend to the mid-cavity and may not be central, with one side being bigger than the other . Women with subseptate or septate wombs are more likely to have difficulties with conception. There is also an increased risk of early miscarriage and preterm birth. In later pregnancy, the baby may not be lying in a head-down (cephalic) position as there is less room for it to move.
Arcuate uterus
The arcuate uterus is the most common type of uterine anomaly, and the mildest form of defect in that it looks very similar to a normal womb from the outside but it has a concave contour at the top and a wider cavity. It has even been described as a normal variant of uterine anatomy. Having an arcuate uterus doesn’t increase your risk of preterm birth or early miscarriage, and most women successfully carry a baby to term. However, some studies have linked an arcuate uterus with a very small risk of late miscarriage, though there is a lack of consensus and many publications have described no association with poor pregnancy outcome.
Most women don’t know that they may have an abnormally-shaped uterus when they become pregnant as it’s unlikely that they will have any physical symptoms in early pregnancy. You might only find out if you have difficulty conceiving or when you have an ultrasound scan after experiencing a miscarriage Some women may find out about the uterine abnormality if they’ve previously had investigations after recurrent miscarriage or gynaecological problems such as abnormal bleeding, or if they come for a private reassurance scan in early pregnancy. The pregnancy can be seen developing in either the right or left horn, or moiety. Sometimes, women with a bicornuate uterus may experience a small amount of vaginal bleeding in early pregnancy, because the hormones cause the lining of the womb (endometrium) in the opposite horn to thicken and bleed.
If you have a didelphic (double) womb or a unicornuate womb, it may be identified during routine pregnancy scans at 12 and 20 weeks. However, pregnancy scans at this later stage may not identify milder forms of womb abnormality. A transvaginal scan in the earlier stages of pregnancy or as part of a gynaecological examination will demonstrate milder forms of the abnormality. Other investigations can include a hysteroscopy, a laparoscopy or a three-dimensional pelvic ultrasound scan.
A hysteroscopy is a procedure to examine the inside of the uterus. It involves placing a small camera through the cervix into the womb cavity. Fluid is flushed inside the womb to allow a view of the whole uterine cavity. During this procedure, the doctor can look at the shape of the womb as well as any other abnormalities such as fibroids or polyps.
If you have had recurrent early miscarriages (3 or more) or one or more second trimester miscarriage, your doctor may suspect that you have an abnormally-shaped womb. They may offer you a pelvic ultrasound or MRI (Magnetic Resonance Imaging) scan to look at the shape of the uterus. Sometimes, a HyCoSy (Hysterosalpingo Contrast Sonography) test might be offered if you are undergoing fertility investigation. This is when liquid is injected through the cervix and pictures are taken using ultrasound to see the flow of the fluid around the womb and fallopian tubes. A Hystero-salpingogram (HSG) might also be useful to look at the shape of the uterine cavity and the fallopian tubes. This uses X-rays to detect a radio-opaque fluid which is injected through the cervix into the uterine cavity. A pelvic ultrasound uses high frequency sound waves to view the uterus. A transvaginal ultrasound scan is preferred as the sound waves are closer to the pelvic organs and a clearer view is obtained. Some hospitals are able to offer 3D transvaginal ultrasound scans which builds up a 3D picture of the shape of the uterine cavity to accurately assess it’s shape.
A laparoscopy may be offered by a gynaecologist, and this is a surgical procedure that allows a surgeon to access the inside of the tummy cavity. A camera is inserted through the abdominal wall to view the uterus, Fallopian tubes and ovaries, but it will only look at the uterus from the outside, and the cavity is not investigated.
The treatment depends on the type of abnormality that you have. Although surgery might sound like a good plan, operations can sometimes lead to further problems which might affect fertility and pregnancy. A gynaecologist will usually discuss any treatment options with you if a congenital uterine abnormality is identified before a pregnancy.
If you are diagnosed with an abnormally-shaped womb during pregnancy, you will be put into the care of an obstetric team. You will have extra scans and hospital visits to check up on you and your baby throughout the pregnancy.
If your baby ends up lying in an awkward position, such as transverse lie (lying across your womb) or breech (bottom first) in later pregnancy, your antenatal team will talk to you about your birth options. They will recommend that you have a Caesarean section, but it is your decision.
If you know you have a uterine abnormality, you may feel anxious during your pregnancy, especially if you’ve previously had a miscarriage or premature baby. It’s important to talk to your midwife about any anxiety you might have, and go to all your antenatal appointments so you can have all the relevant tests and scans. It’s also good to know the signs and symptoms of pre-term labour, just in case your baby arrives early.
