Background
Uterus Didelphys is a congenital malformation of the
Mullerian duct that occurs because of complete failure of
fusion of the ispilateral ducts. It results in the developments of
a longitudinal vaginal septum, two vaginas, and two hemi-uteri
each with its separate ovary and fallopian tube. The incidence
of this anomaly is 1 in 3000 [1]. It remains a challenge to the
obstetricians especially when it is undiagnosed before onset of
labor. Patients are usually asymptomatic, but the anomaly may
be associated with dysmenorrhoea, dyspareunia, infertility,
spontaneous abortion, preterm labor, fetal malpresentation,
intrauterine growth restriction, PROM, renal agenesis, decreased
live births and caesarean delivery [1-6].
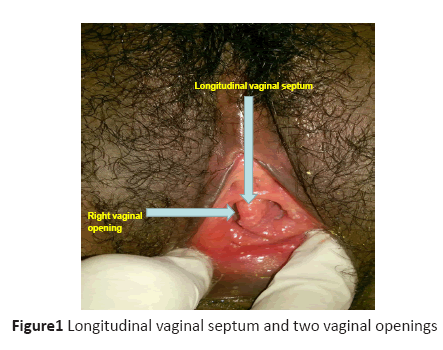
Diagnosis is usually initiated by the findings of a
longitudinal vaginal septum and two vaginal openings during
a vaginal examination. A 3-D transvaginal sonography is an
excellent non-invasive method of investigation [6]. Others
methods of investigations include sonohysterography,
hysterosalpingography, hysterolaparoscopy and pelvic magnetic
resonant imaging. The incidence of caesarean delivery in uterus
Didelphys in pregnancy may be as high as 82% [2]. Several
good pregnancy outcomes including vaginal deliveries, twin
and triplet pregnancies have, however, been reported [7-11].
The aim of this case report is to make clinicians to have high
index of suspicion of uterine anomaly when investigating
cases of dysmenorrhea, dyspareunia, infertility, spontaneous
abortion, preterm labor, fetal malpresentation, intrauterine
growth restriction, PROM, and renal agenesis. Early diagnosis,
meticulous follow up can avert most of these complications
We present a case report of an undiagnosed uterus Didelphys
in term pregnancy that was complicated with prolonged PROM, intrauterine fetal death, failed induction of labor, and
an emergency caesarean delivery to buttress the need for early
diagnosis, close monitoring in pregnancy and labor to avert
adverse outcomes.
Case report
Miss OE was 32-year-old Gravida2 Para0+1 office attendant.
She was referred to ESUTH, Enugu on 11/11/2015 for
prolonged rupture of fetal membranes, and intrauterine fetal
death. She attained menarche at 15 years and had a regular 28-
days cycle with 4 days normal menstrual bleeding. There was
neither history of infertility nor dysparenuia. She had medical
abortion of a confirmed-seven-week unwanted pregnancy in
2013 without complications.
She booked for antenatal care in the index pregnancy in
the referral hospital at GA of 26weeks. She complied with
her antenatal appointments, investigations and drugs. There
was no history of threatened abortion or preterm contractions.
She received two tetanus toxoid injections and anti-malarial
prophylaxis at the 24th and 30th week’s gestation respectively.
The pregnancy was uneventful until 41 weeks plus 6 days when
she had PROM. She presented to the referral hospital where
she was observed for 24 hours, had two vaginal examinations,
and was later discharged without augmentation of labor. About
thirty hours later she represented to the same hospital with mild
uterine contractions, and was then referred.
There were mild uterine contractions at presentation. She
was not pale. The pulse rate was 110 beats per minute, and
blood pressure was 120/80mmHg. Her respiratory rate was 18
cycles per minute. The symphysiso-fundal height corresponded
to 39weeks intrauterine pregnancy, the fetal lie was longitudinal with 5/5 cephalic presentation. The fetal heart sounds were not
heard. Initial vaginal examinations and an abdominal ultrasound
missed the diagnosis of uterus Didelphys. She had intravenous
Ceftriaxone 1g 12 hourly, and metronidazole 500mg 8hrly for
48 hours. Vaginal misoprostol 50 micro grammes were inserted
6 hourly x 4 without significant cervical changes. A diagnosis
of failed induction was made and patient was booked for an
emergency caesarean delivery. Her bedside clotting time was 5
minutes before the surgery. A critical review of the patient before
surgery showed a longitudinal vaginal septum, two vaginal
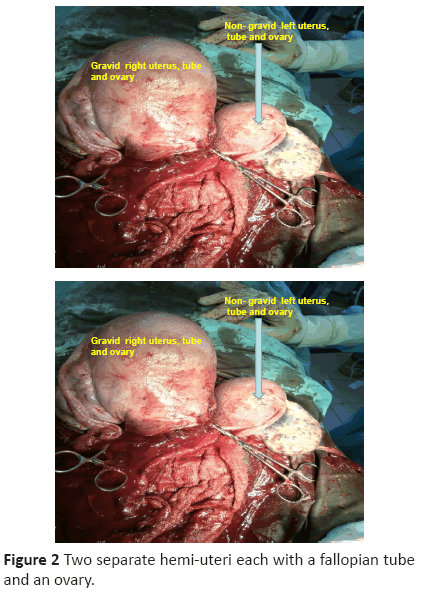
openings, and uterus Didelphys was confirmed at surgery as
shown in figures 1 and 2. (Figure1), (Figure 2).
Figure 1: Longitudinal vaginal septum and two vaginal openings
Figure 2: Two separate hemi-uteri each with a fallopian tube
and an ovary.
There were a gravid right uterus and a non gravid left
uterus measuring 11cm X 6cm occupying the pelvis. Each
uterus has its separate ovary and fallopian tube. A macerated
male baby that weighed 3.2kg was delivered. Estimated blood
loss was 1litre. She had 2 units of blood intra-operative. The
postoperative recovery was uneventful. She was discharge on
the 7th postoperative day after counseling her on family planning
and how to manage her subsequent pregnancies. She opted for
interval CuT380A intrauterine device at six week postnatal visit.
Discussion
Uterus Didelphys is rare and sometimes not even diagnosed. It
occurs in 0.1% -0.5% of healthy fertile population [12]. Heinonen
PK (2000) [3], evaluated the long-term clinical consequences, and
reproductive performances of 49 women with uterus Didelphys that
were followed up to 6.3 years. He found obstructed hemi vagina
in 9 (18%) with 8 (16.3%) having ipsilateral renal agenesis. Five
(13%) had primary infertility. Thirty four out of 36 (94%) women
who wanted to conceive became pregnant, 21% had miscarriage
while 2% were ectopic pregnancy. The fetal survival rate was 75%,
prematurity 24%, fetal growth retardation 11%, perinatal mortality
5.3%, and caesarean delivery rate 84%. Pregnancy was located in
the right uterus in 76% cases. Miss OE did not experience most of
these complications associated with uterus Didelphys. Many of the
patients with uterus Didelphys have normal sex lives, pregnancies,
and deliveries [11]. Miss OE pregnancy was in the right uterus,
and remained uneventful until she had prolonged term PROM,
intrauterine fetal death, failed induction of labor and an emergency
caesarean delivery. Her uterus Didelphys was undiagnosed until
she was critically reviewed for failed induction. She missed the meticulous prenatal care that was advocated by Heine on PK (2000) [3] that would have prevented the adverse outcomes that
were associated with this anomaly. Early diagnosis and prompt
operative delivery would have prevented the fetal death in Miss
OE. She had primary postpartum hemorrhage (>1 liter) due
to uterine agony at surgery, and was transfused 2 units of blood
intra-operative. CuT380A was not inserted during the emergency
caesarean delivery to allow adequate treatment of uterine infection.
Previous studies including this study were mostly case reports, and
the results cannot be generalized on the general population. Only
Heinonen PK (2000) [3], was able to follow 49 cases up to 6.3
years. Recent advances in diagnostic techniques, and availability
of meticulous medical services and treatments for the associated
complications that favor good outcomes depict the international
clinical relevance of early diagnosis of the subject. None availability
of such modern diagnostic technique in most developing countries
like Nigeria may be the cause of the delay in establishing diagnosis,
and thus delayed prompt interventions in Miss OE that could have
averted the adverse fetal outcome. The directions for further studies
should include universal availability of diagnostic techniques like
3 D ultrasound with vaginal probes so that population study can
be undertaken, uterine anomalies identified, and protocol for the
management such anomalies established.
Conclusion
Clinicians should have high index of suspicion of uterine
anomaly to make early diagnosis of uterus Didelphys. Pregnancy
in a uterus Didelphys deserves early diagnosis of the anomaly,
and meticulous care in pregnancy and delivery to avert the
associated adverse outcomes.
References
- Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Dervoey P (2001) Clinical implications of uterine malformation and hysterscopic treatment results. Hum Reprod Update 7: 161-174.
- Heinonen P K (1984), “Uterus didelphys: a report of 26 cases,” European Journal of Obstetrics & Gynecology and Reproductive Biology, vol. 17, no. 5, pp. 345–350.
- Heinonen PK (2000), “Clinical implications of the didelphic uterus: long-term follow-up of 49 cases,” European Journal of Obstetrics & Gynecology and Reproductive Biology, vol. 91, no. 2, pp. 183–190.
- Raga F, Bauset C, Remohi J, Bonilla-Musoles F, Simon C, and Pellicer A,(1997) “Reproductive impact of congenital Mullerian anomalies,” Human Reproduction, vol. 12, no. 10, pp. 2277–2281.
- Acien P (1993), “Reproductive performance of women with uterine malformations,” Human Reproduction, vol. 8, no. 1, pp. 122–126.
- Madureira AJ, Mariz CM, Bernardes JC, Ramos IM (2006). Case 94: Uterus Didelphys with Obstructing Hemivaginal Septum and Ipsilateral Renal Agenesis. Radiology 239: 602-606.
- C. Magudapathi (2012). “Uterus didelphys with longitudinal vaginal septum: normal deliver—case report,” Journal of Clinical Case Reports, vol. 2, article 13.
- R. Garg, A. Kwatra, and V. Bangal, “A rare case of uterus didelphys with full term pregnancy in each horn,” Pravara Medical Review, vol. 2, no. 4, pp. 22–24, 2010.
- Mashiach S, Ben-Rafael Z, Dor J, Serr DM (1981) Triplet Pregnancy in Uterus Didelphys with Delivery Interval of 72 days. Obstet Gynecol 58: 519-521.
- Magudapathi C (2012), Uterus Didelphys with Longitudinal Vaginal Septum: Normal Delivery. Journal of Clinical Case Reports. 2:13 https://dx.doi.org/10.4172/2165-7920.1000194.
- Mohd Subhail, Hina Khan, Sofia Suhail (2010). Uterus Didelphys having Single Pregnancy in her right horn: A Case Report. Journal of Chinese Clinical Medicine Volume 5 (1): 46-49.
- Green LK, Harris RE (1976).Uterine anomalies; frequency of diagnosis, and obstetric complications, 47 (4):427-428.