Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Huvila J, Gilks CB. Benign, borderline and malignant Brenner tumors. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorb9brenner.html. Accessed May 6th, 2024.
Definition / general
- Tumor composed of transitional / urothelial-like epithelium, typically embedded in fibromatous stroma
- Benign, borderline and malignant variants are recognized, based on the growth pattern and cytological features of the epithelial cells
Essential features
- Benign Brenner tumor:
- Adenofibromatous architecture with nests of bland transitional epithelium present within fibromatous stroma
- Borderline Brenner tumor:
- Papillary architecture with papillae covered by multilayered transitional epithelium
- There is variable but usually low grade cytological atypia
- Malignant Brenner tumor:
- Stromal invasion by carcinoma with transitional cell features, associated with a benign or borderline Brenner tumor
ICD coding
- ICD-O:
- ICD-11:
- 2F32.Y & XH5DX3 - Brenner tumor, NOS
- 2C73.Y & XH2CH8 - Brenner tumor, borderline malignancy
- 2C73.Y & XH6NJ7 - Brenner tumor, malignant
Epidemiology
- Brenner tumors are most common in the fifth and sixth decades but can occur across a wide age range
Sites
- Ovary
- Rare extraovarian Brenner tumors are reported
Pathophysiology
- Cell of origin of Brenner tumors is controversial; they may arise from Walthard rests
Etiology
- Unknown
Clinical features
- Benign Brenner tumors are usually asymptomatic
- Borderline and malignant Brenner tumors are larger and usually present with findings secondary to an adnexal mass
Diagnosis
- Most benign Brenner tumors are an incidental finding in an ovary removed for other reasons
- Borderline and malignant Brenner tumors are usually diagnosed at the time of removal of an adnexal mass
Radiology description
- Nonspecific findings of a solid or solid and cystic ovarian mass
Prognostic factors
- All reported cases of benign and borderline Brenner tumor have had a benign course, although local recurrence has rarely been reported for the latter (Acta Pathol Microbiol Scand Suppl 1972;233:56)
Case reports
- Benign Brenner tumor:
- 58 year old woman with a coexisting benign Brenner tumor and mucinous cystadenoma (Iran J Pathol 2020;15:334)
- 60 year old postmenopausal woman with ovarian mucinous cystic tumor associated with sarcomatous mural nodule and benign Brenner tumor (Medicine (Baltimore) 2019;98:e14066)
- 68 year old woman with a benign Brenner tumor arising in an ectopic ovary (Int J Gynecol Pathol 2020 Sep 17 [Epub ahead of print])
- Borderline Brenner tumor:
- 68 year old woman with borderline Brenner tumor (J Ovarian Res 2014;7:101)
- Malignant Brenner tumor:
- 62 year old woman with malignant Brenner tumor manifesting as bowel obstruction (BMJ Case Rep 2020;13:e235394)
- 77 year old woman with malignant Brenner tumor (Gynecol Oncol Rep 2017;22:26)
Treatment
- Oophorectomy
- No adjuvant treatment for benign or borderline Brenner tumors
- Adjuvant chemotherapy for advanced stage malignant Brenner tumors
Gross description
- Benign Brenner tumor:
- Small (usually < 2 cm), circumscribed, fibrous tumor with a uniform cut surface
- Calcifications may be present
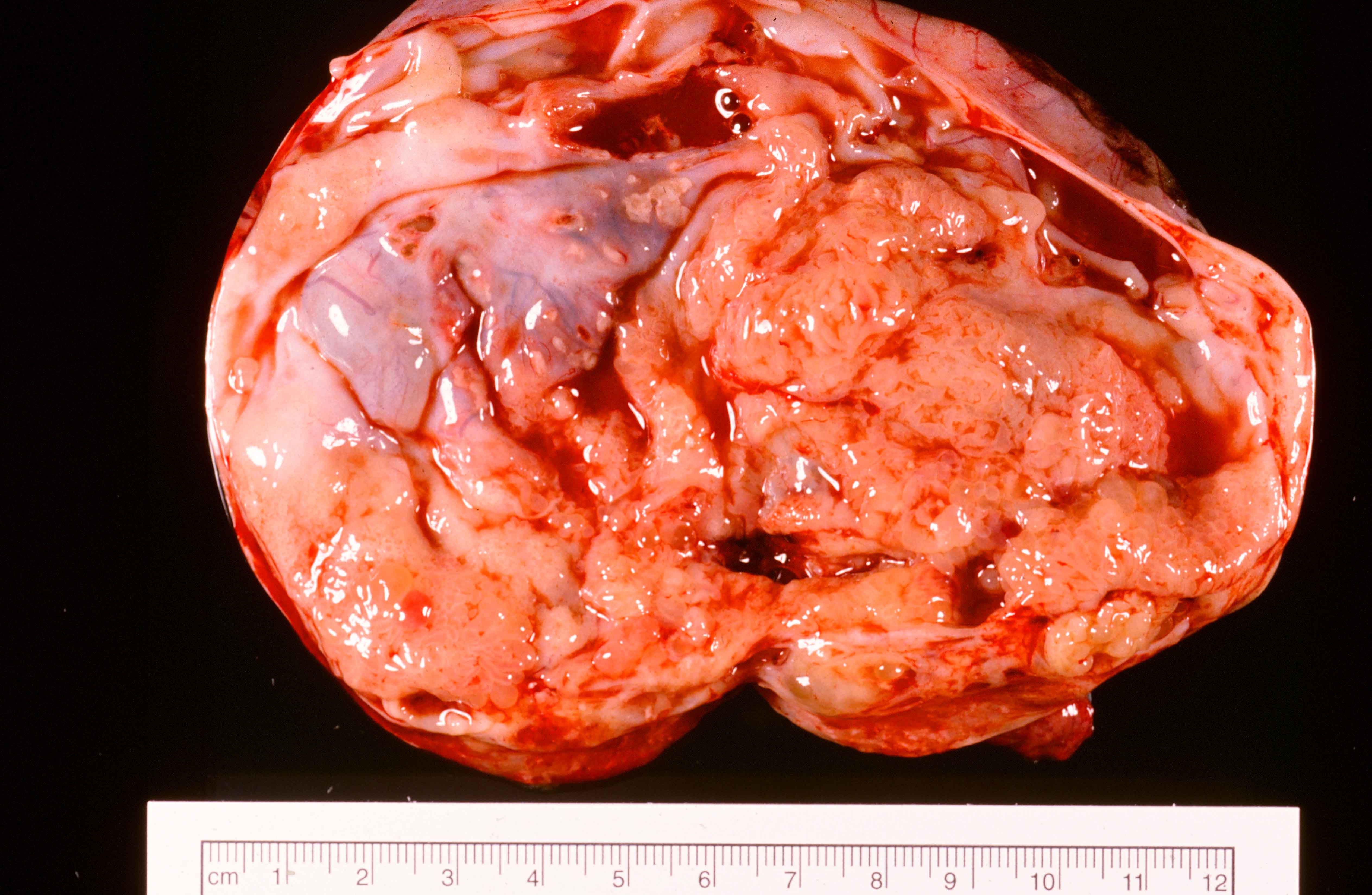
- Borderline and malignant Brenner tumor:
- Smooth surface, larger (usually > 10 cm) with fleshy, polypoid masses projecting into cystic cavity(s)
Gross images
Frozen section description
- Benign:
- Adenofibromatous architecture, smooth contoured nests of bland epithelial cells within benign fibromatous stroma
- Borderline or malignant:
- Resembling low grade papillary urothelial tumor of the bladder, with papillary fronds covered by transitional-like epithelium
Frozen section images
Microscopic (histologic) description
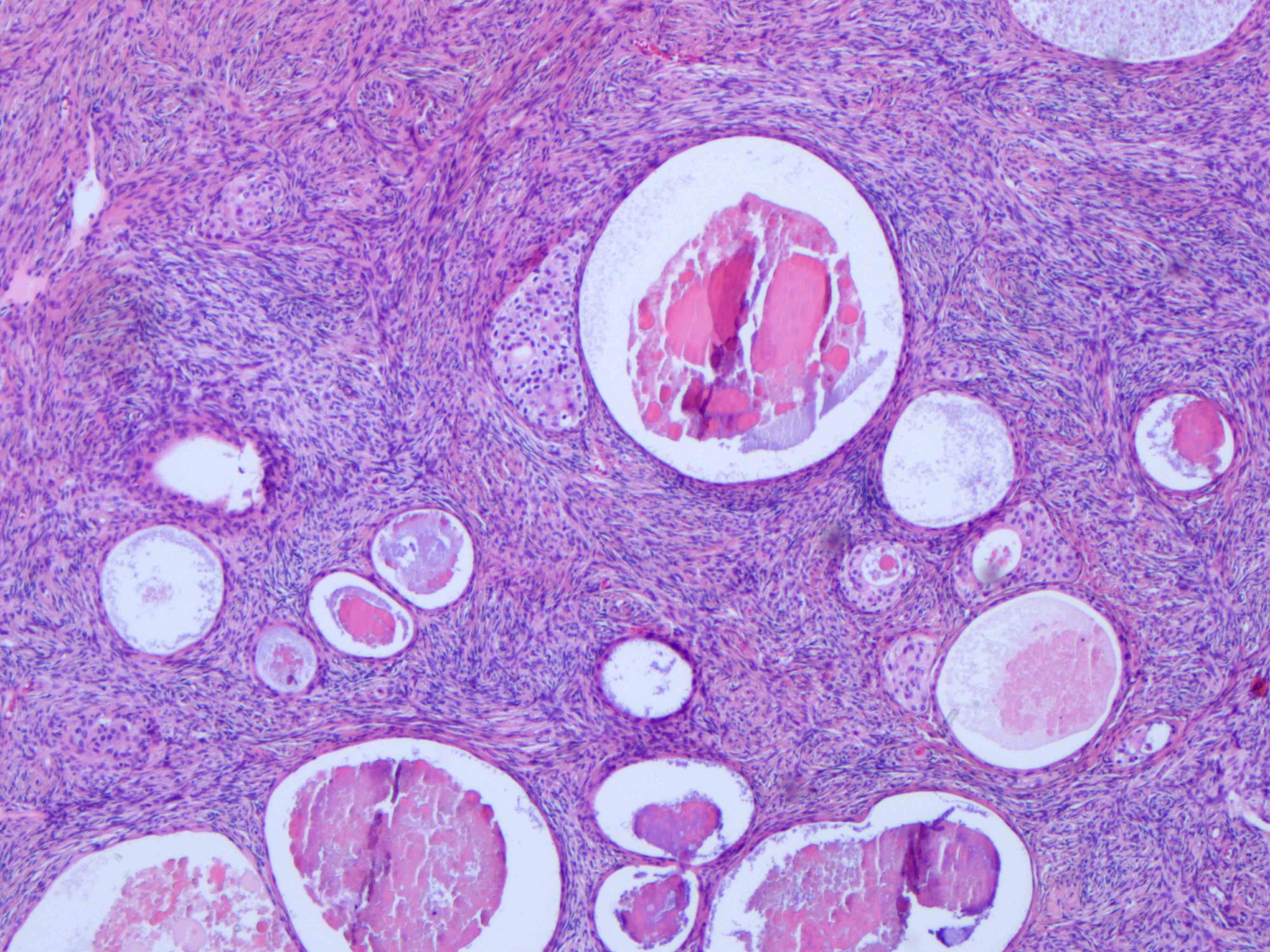
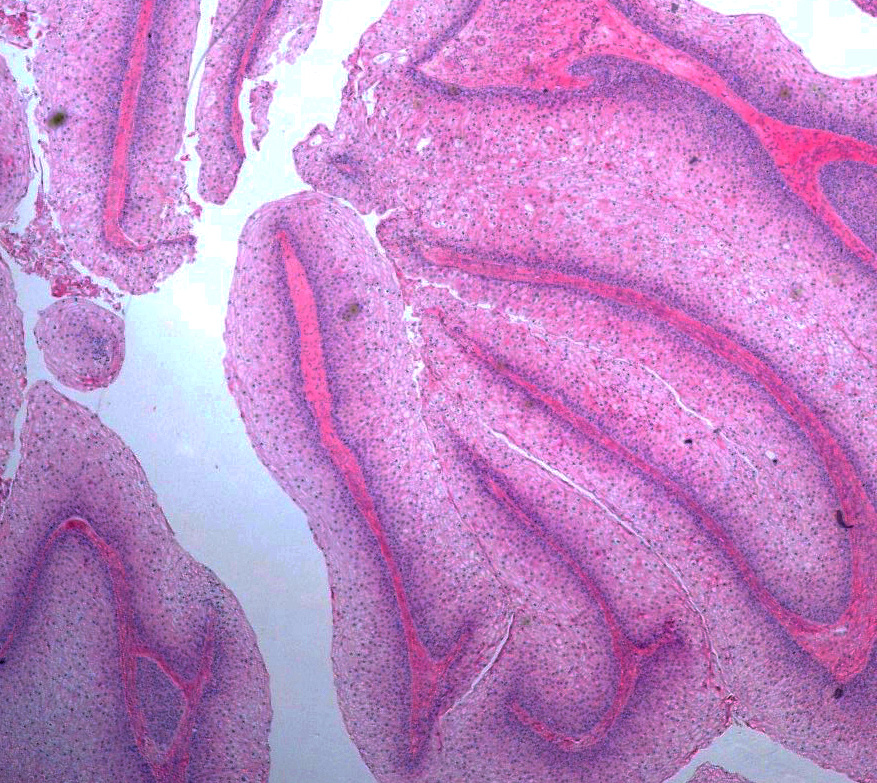
- Benign:
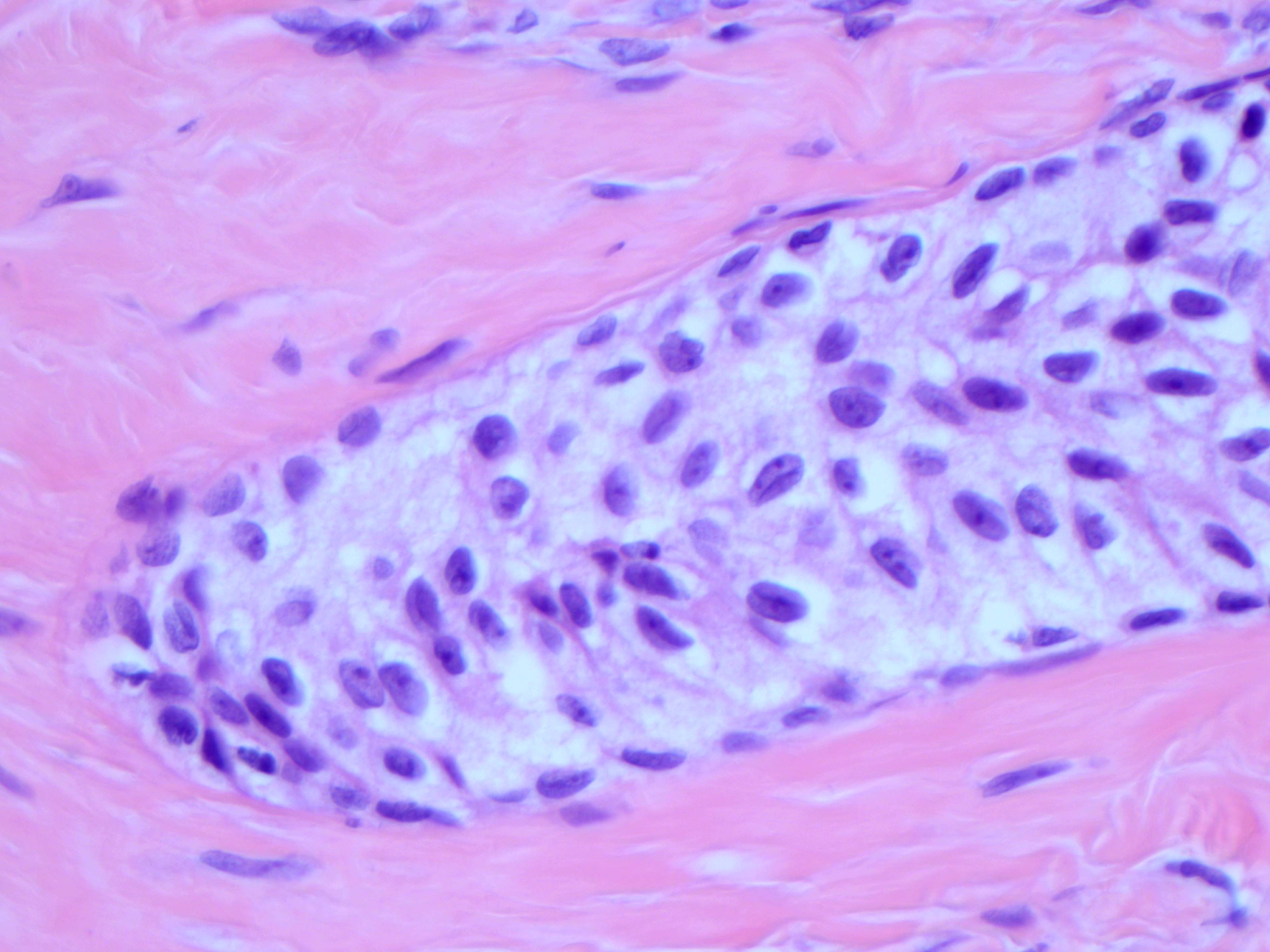
- Smooth contoured nests of bland transitional epithelium within fibromatous stroma
- Transitional cells have uniform oval nuclei and may have a longitudinal nuclear groove
- There may be mucinous epithelium at the center of the nests, with microcyst formation
- Ciliated or nondescript glandular epithelium may be present; a coexistent mucinous cystadenoma is present in 10% of cases
- Calcification is common
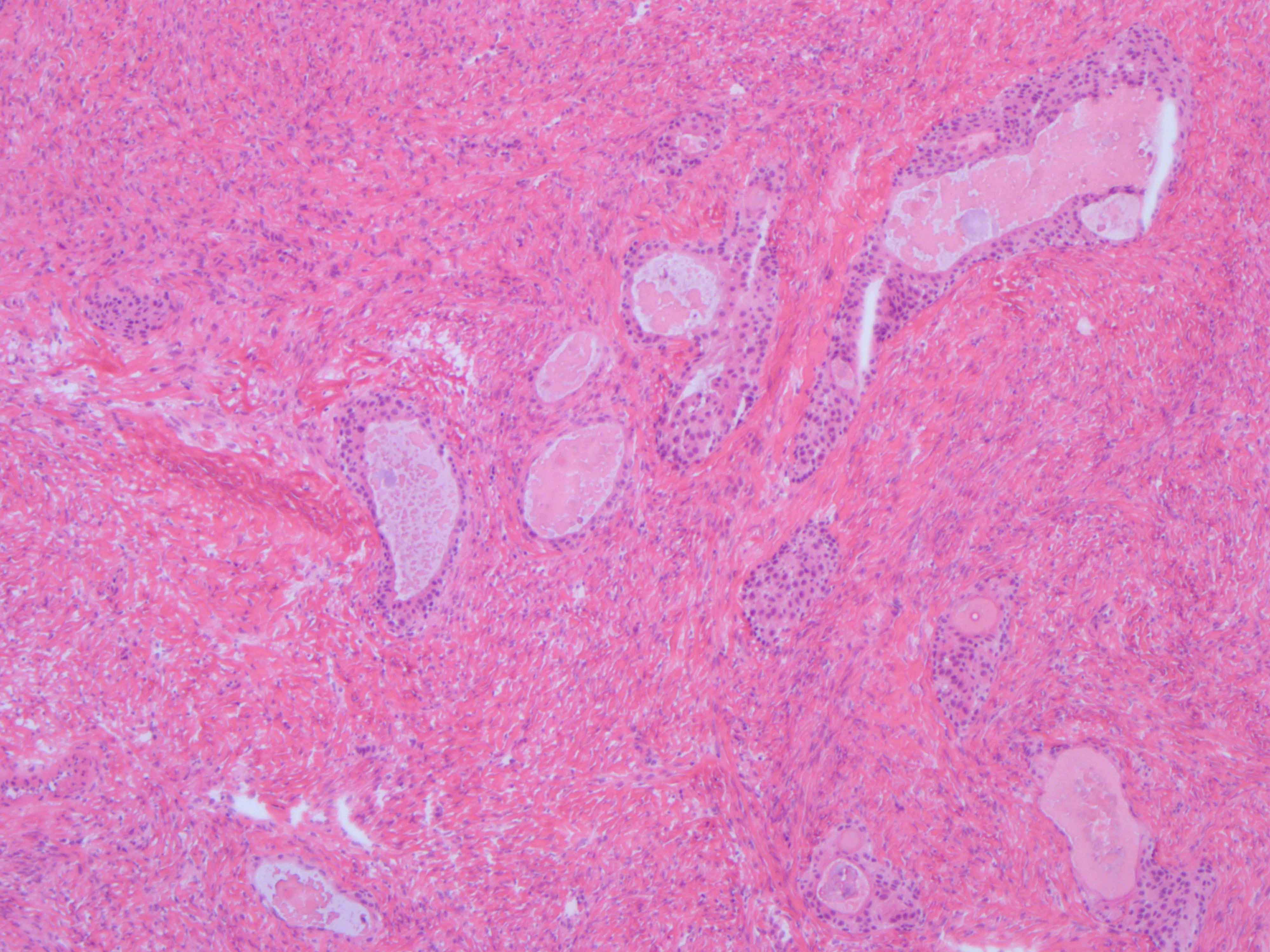
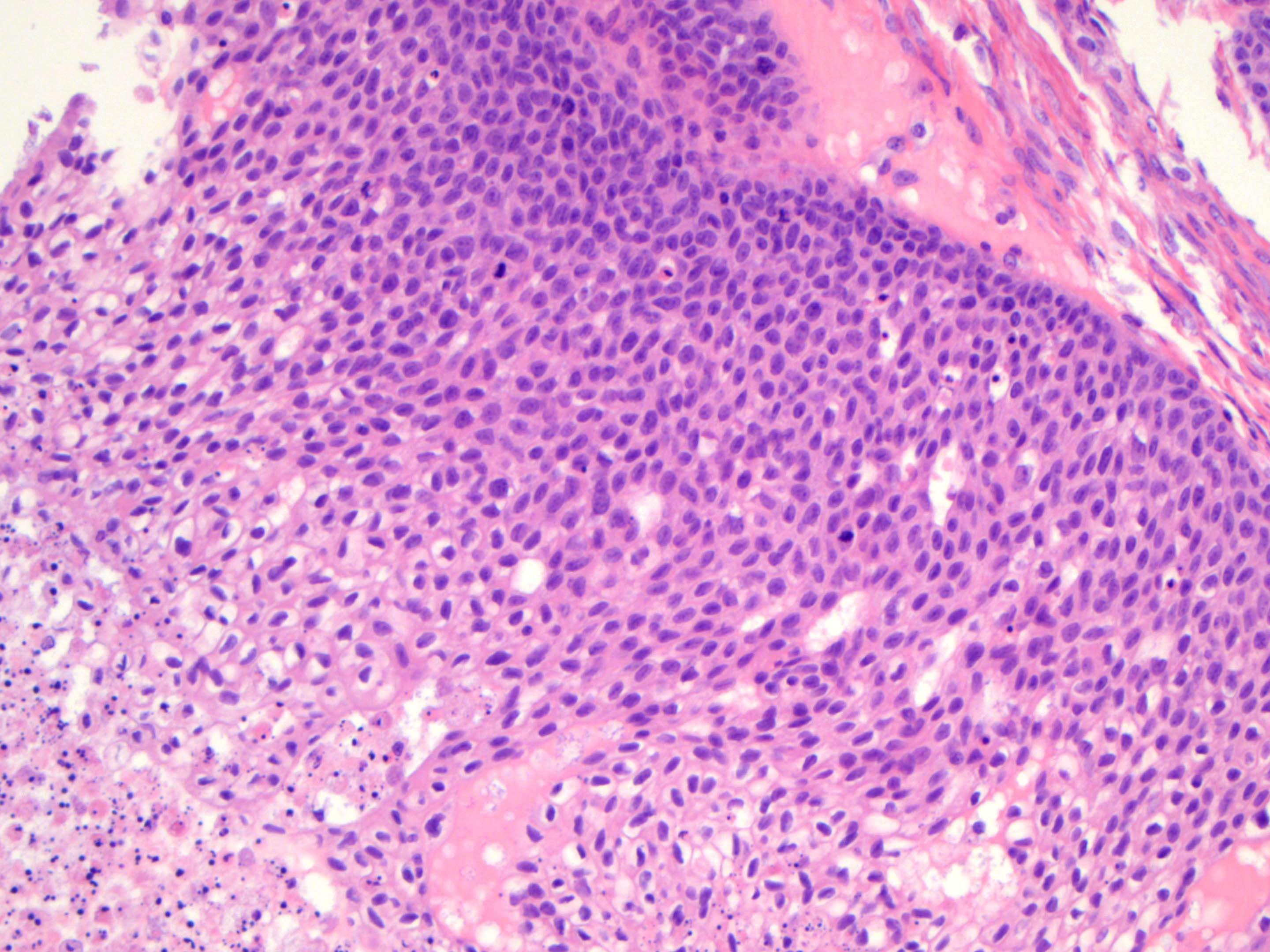
- Borderline:
- Papillary architecture with papillae covered by multilayered transitional epithelium
- There is variable cytological atypia; usually low grade but on occasion moderate or marked cytological atypia may be present
- Benign Brenner tumor component is often present
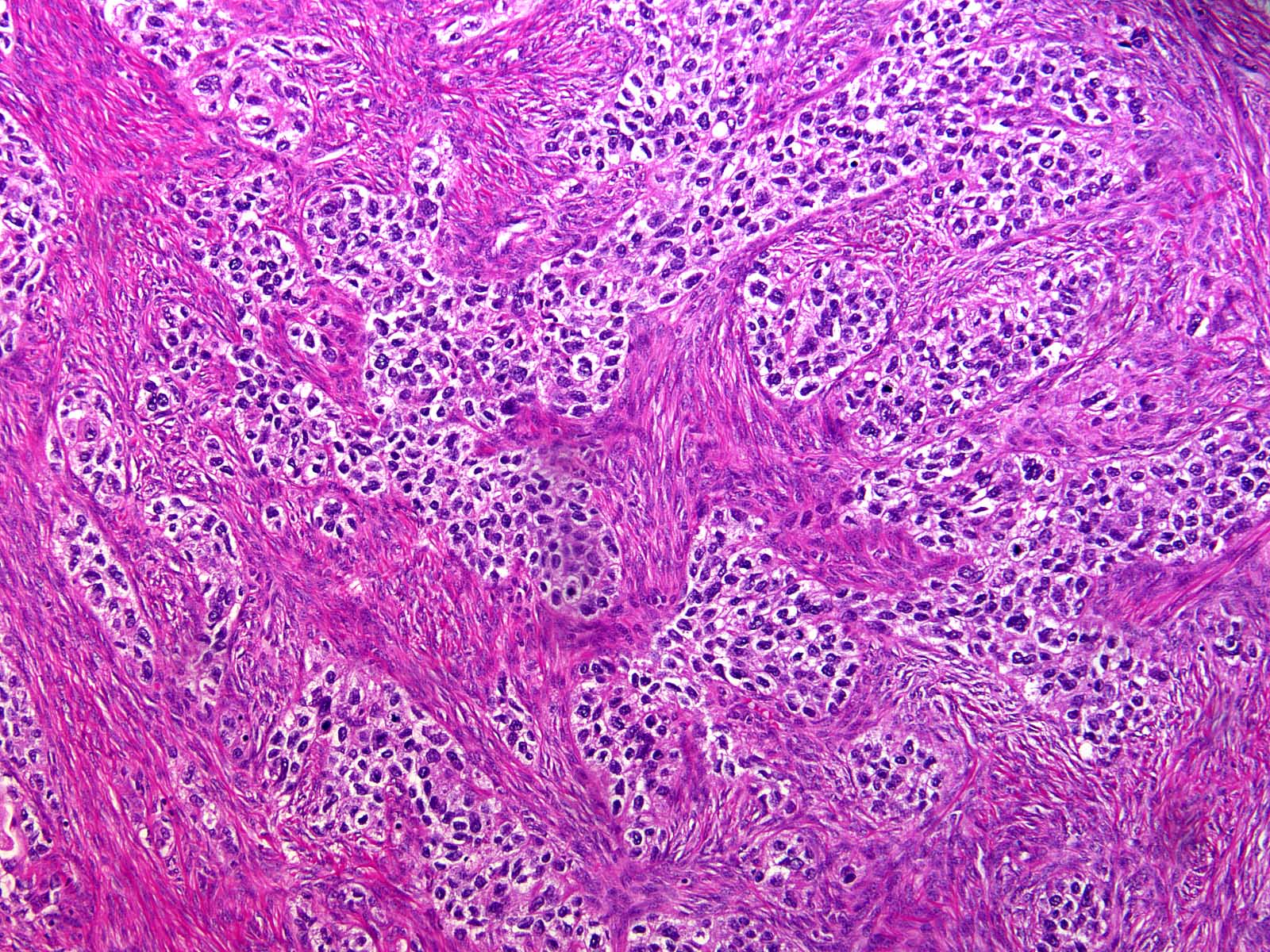
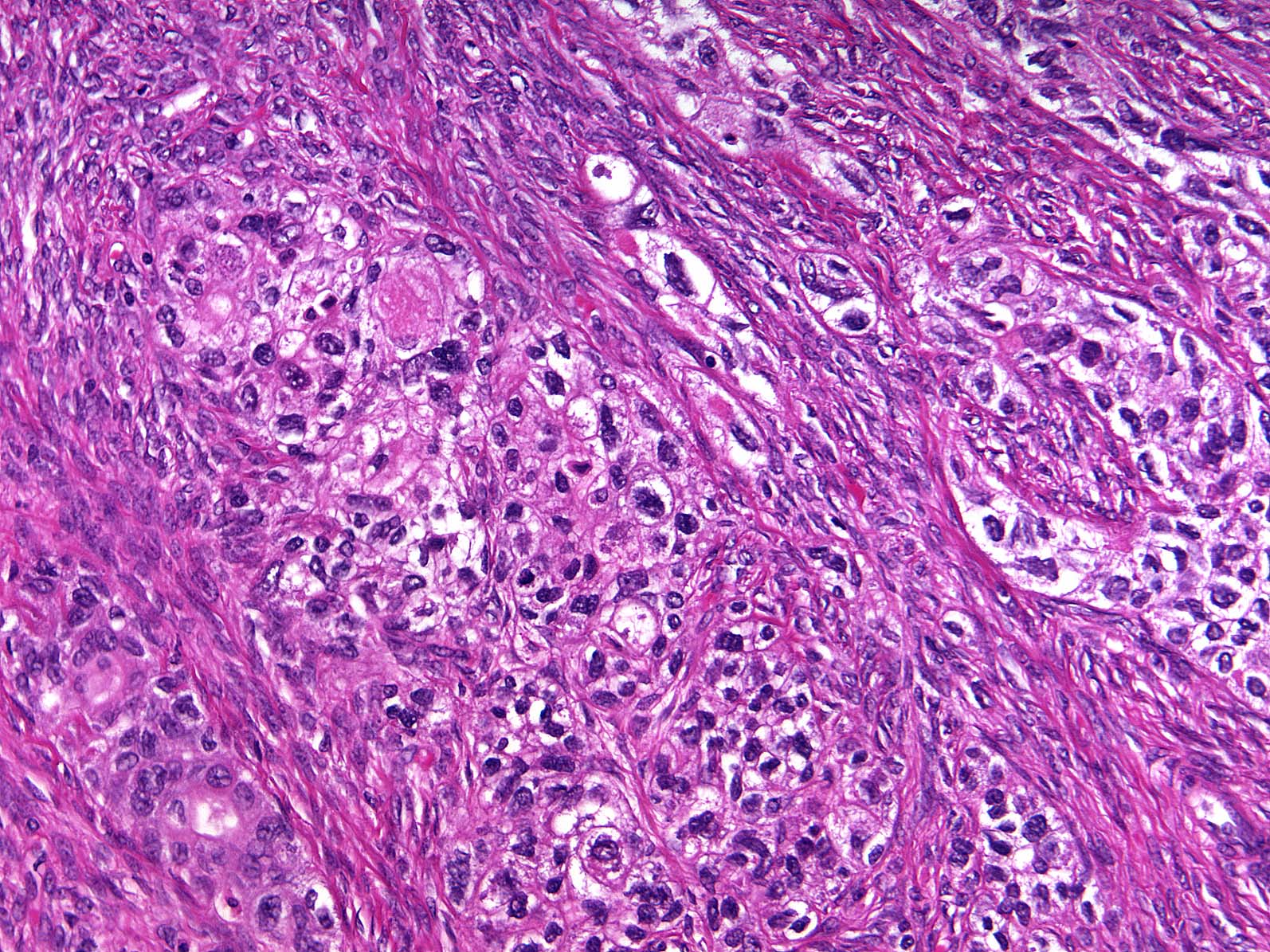
- Malignant:
- Stromal invasion by carcinoma with transitional cell features, with irregular nests of cells and single cells in an infiltrative pattern
- Squamous or mucinous differentiation may be present
- Benign or borderline Brenner tumor component is present
- Reference: Int J Gynecol Pathol 2012;31:499
Microscopic (histologic) images
Contributed by Jutta Huvila, M.D., Ph.D. and C. Blake Gilks, M.D.
AFIP images
Positive stains
Negative stains
Sample pathology report
- Right ovary, oophorectomy:
- Borderline Brenner tumor (see comment)
- Comment: This borderline Brenner tumor is associated with a component of benign Brenner tumor. Negative for invasive carcinoma.
Differential diagnosis
- For Benign Brenner tumor
- Endometrioid adenofibroma:
- Glandular: lacks multilayered epithelial nests with transitional differentiation
- Adult granulosa cell tumor:
- More characteristic patterns of adult granulosa cell tumor present, such as microfollicular, trabecular or solid growth
- Inhibin immunoreactivity and negative for epithelial markers
- Carcinoid tumor:
- Insular or trabecular architecture
- Lacks prominent fibromatous stroma
- Expression of neuroendocrine markers
- Endometrioid adenofibroma:
- For borderline / malignant Brenner tumors
- High grade serous carcinoma, transitional architectural pattern:
- Areas of conventional high grade serous carcinoma
- High grade nuclear features
- Absence of a benign Brenner component
- WT1 and ER positivity (Int J Gynecol Pathol 2012;31:49)
- Squamous cell carcinoma:
- Keratinization
- High grade cytological features
- Teratoma component
- Endometrioid borderline tumor or carcinoma:
- More prominent glandular component with endometrioid (not mucinous) glands
- ER positive
- Metastatic squamous cell carcinoma:
- History of primary squamous cell carcinoma elsewhere in the body
- Bilateral and multinodular growth
- Lacks prominent papillary architecture
- Metastatic urothelial carcinoma:
- History of urothelial carcinoma
- Bilateral and multinodular growth
- Lacks benign Brenner component
- High grade serous carcinoma, transitional architectural pattern:
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Brenner tumors of the ovary typically have which of the following immunophenotypes?
- GATA3 and ER positive
- GATA3 and p63 positive
- GATA3 and WT1 positive
- GATA3 positive and mutant pattern p53 expression
Board review style answer #2