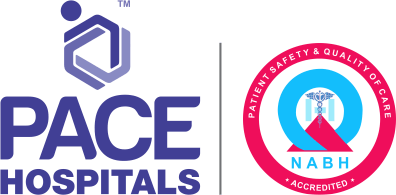
Celiac Disease Symptoms, Causes, Risk Factors and Complications
Celiac disease meaning
Celiac disease, commonly known as "gluten-sensitive enteropathy," is a small intestine autoimmune disease where the body's immune system reacts inappropriately to consumed gluten (a protein found in barley, rye, and wheat), resulting in small intestine inflammation and damage. This is a chronic condition, and patients with celiac disease can present with severe diarrhoea and failure to thrive, and some may be asymptomatic.
Celiac disease affects roughly 0.5 -1 % of the overall population. People suffering from autoimmune diseases, such as Addison's disease, type 1 diabetes, and microscopic colitis, have a higher risk. Avoid eating anything containing gluten is the only cure for celiac disease. The risk for nutritional deficiency and complications of celiac disease, as well as the required degree and duration of adherence to a gluten-free diet, can be identified by distinguishing between celiac disease and non-celiac gluten sensitivity.
Celiac disease causes
An individual with HLA-dominant DQ2 or DQ8 genes who is genetically predisposed has a higher chance of developing Celiac disease. The other possible contributors include infant feeding methods, gastrointestinal illnesses, and gut microorganisms. Surgery, pregnancy, childbirth, a virus (enterovirus and adenovirus infections), or extreme emotional stress can sometimes activate the celiac disease.
The condition is caused by the immune system's abnormal reaction to gluten. The glycoprotein gliadin (found in gluten) directly harms enterocytes (cells of the intestine) via increasing IL-15 production, leading to inflammation and the destruction of small intestinal villi.
Vili (a finger-like projection) presents in the inner lining of the small intestine and aids in the absorption of nutrients. The destruction of small intestinal villi results in diminished gut surface functionality and malabsorption. The lack of nutritional absorption has an immediate influence on the digestive system, in addition to an indirect impact on all of the body's systems.
Celiac disease symptoms
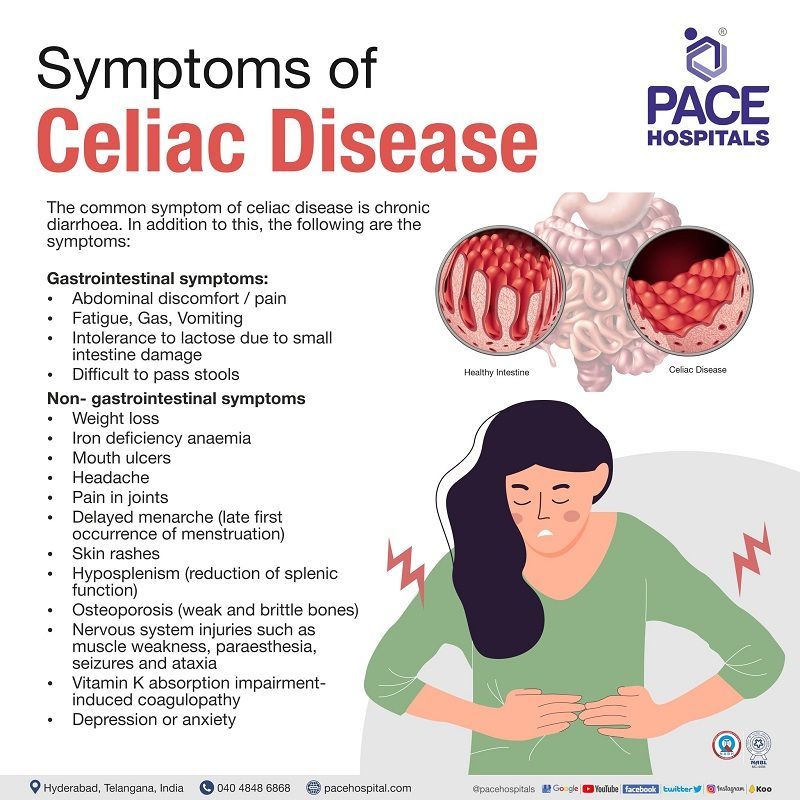
The common symptom of celiac disease is chronic diarrhoea (loose, watery, frequent bowel moments). In addition to this, the following are the symptoms:
Gastrointestinal symptoms:
- Abdominal discomfort/pain
- Fatigue
- Gas
- Vomiting
- Intolerance to lactose due to small intestine damage
- Difficult to pass stools
Non- gastrointestinal symptoms
- Weight loss
- Iron deficiency anaemia
- Mouth ulcers
- Headache
- Pain in joints
- Delayed menarche (late first occurrence of menstruation)
- Skin rashes
- Hyposplenism (reduction of splenic function)
- Osteoporosis (weak and brittle bones)
- Nervous system injuries such as muscle weakness, paraesthesia, seizures and ataxia
- Vitamin K absorption impairment-induced coagulopathy
- Depression or anxiety
Celiac disease symptoms in children
- Difficult to pass the stools
- Gas
- Chronic diarrhoea
- Delayed puberty
- Foul smelling stools
- Nausea & vomiting
- Abdominal swelling
- Loss of weight
- Anaemia
- Damage of tooth enamel
- Failure to thrive in infants
- Low height
- Neurological symptoms include attention-deficit hyperactivity disorder, seizures and lack of muscle coordination
- Irritability
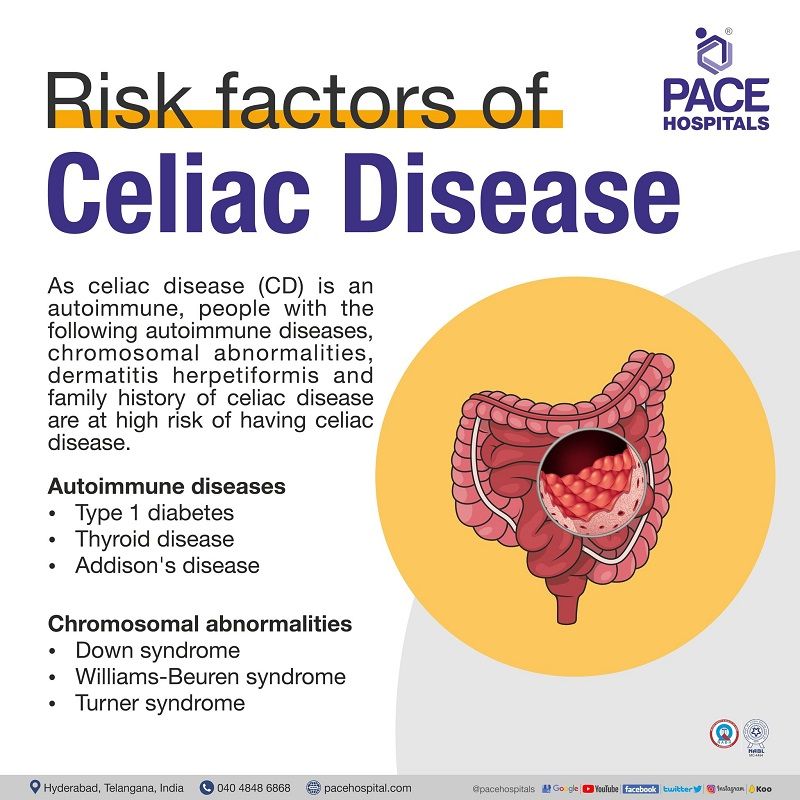
Celiac disease risk factors
As celiac disease (CD) is an autoimmune, people with the following autoimmune diseases and chromosomal abnormalities are at high risk of having celiac disease, such as:
Autoimmune diseases
- Type 1 diabetes
- Thyroid disease
- Addison's disease
Chromosomal abnormalities
- Down syndrome
- Williams-Beuren syndrome
- Turner syndrome
In addition to the above, people with dermatitis herpetiformis and a family history of celiac disease are also at increased risk for celiac disease.
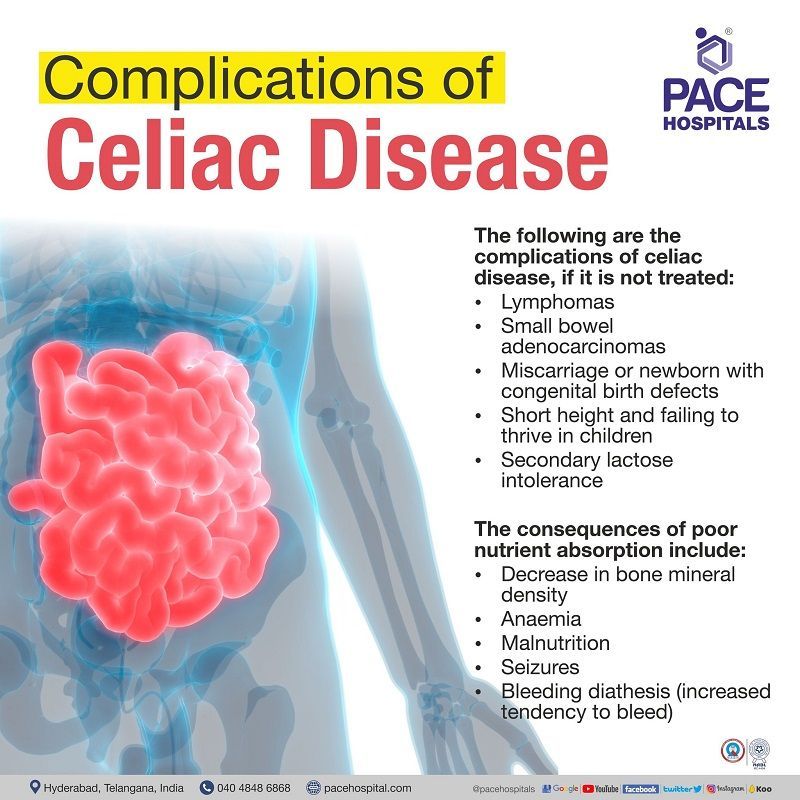
Celiac disease complications
The following are the complications of celiac disease if it is not treated:
- Lymphomas
- Small bowel adenocarcinomas
- Miscarriage or newborn with congenital birth defects
- Short height and failing to thrive in children
- Secondary lactose intolerance
The consequences of poor nutrient absorption include:
- Decrease in bone mineral density
- Anaemia
- Malnutrition
- Seizures
- Bleeding diathesis (increased tendency to bleed)
Celiac disease screening
The celiac disease screening test is beneficial in patients with asymptomatic first-degree relatives of patients with a confirmed diagnosis of celiac disease. Serology tests to check for celiac disease antibodies should be performed on people who exhibit celiac disease symptoms.
Celiac disease diagnosis
The gastroenterologist will perform a physical exam and check the patient's medical and family history to determine the need to go for the following diagnostic tests.
- Serological tests for Immunoglobulin antibodies
- Biopsy of skin in individuals in case of Dermatitis Herpetiformis
- Genetic test
If the serologic tests are positive for celiac disease, the gastroenterologist may recommend further testing such as:
- Endoscopy biopsy of the small intestine
- Capsule endoscopy
Celiac disease treatment
Celiac disease treatment typically entails abstaining from gluten, as onlya strict, lifelong healthy gluten-free diet can aid in controlling the disease. In addition to this, the patient’s symptoms can be managed with gluten-free supplements
- Copper, folate, iron, zinc and vitamin supplements to manage anaemic, malabsorption and malnutrition condition
- Anti-acne agents to manage dermatitis herpetiformis
In addition to the above supplements, anti-inflammatory agents can be prescribed to reduce bowel inflammation.
Foods that contain gluten:
Wheat, barley, and rye are common constituents in various other eatable or consumable products in addition to a daily diet. Additionally, wheat is included as a flavour, colouring, or thickening ingredient. The following foods should be avoided if they are not labelled or mentioned as “gluten-free”.
- Processed foods like Pastas, French fries, Hot dogs and processed lunchmeats
- Liquid or semi-solid foods such as Salad dressings, Beer, Soups, Soya sauces
- Seasoned snack foods
- Crackers and croutons
- Sugar candies
- Cakes
- Cereals
- Seafood or meat flavoured
- Bread
Refractory celiac disease
In some rare instances, even while adhering to a gluten-free diet, symptoms and damage to the small intestine can persist or recur, a condition known as a refractory celiac disease that might cause serious complications such as cancer (T-cell lymphoma) conditions and malnutrition.
Frequently asked questions
-
What can happen if celiac disease goes untreated?
In people with untreated celiac disease, it can lead to the occurrence of other autoimmune disorders, such as multiple sclerosis (MS), Addison's disease, type 1 diabetes (T1DM) etc, and a wide variety of various conditions, including but not limited to anaemia (iron deficiency), dermatitis herpetiformis (an itchy skin rash), decrease in bone density and mass, heart disease, infertility and miscarriage, intestinal cancers, and neurological conditions like migraines, epilepsy, and short stature.
-
Can you die from untreated celiac disease?
While the celiac disease itself is not fatal, the complications that might arise from not treating it can be. These include but are not limited to osteoporosis, chronic anaemia, malnutrition, and an increased risk of acquiring certain forms of cancer.
-
Is there treatment for celiac disease?
Yes, celiac diseases can only be treated by avoiding consuming gluten (protein available in barley, rye and wheat) for the rest of life. In addition to this, the symptoms can be managed by anti-inflammatory agents and gluten-free supplements such as minerals and vitamins.
-
How I knew I had celiac disease?
A person with celiac disease is prone to have gastrointestinal symptoms such as severe diarrhoea, abdominal pain, gas, etc., on a gluten diet. Serologic tests (tTG-IgA, EMA-IgA, DGP-IgA, DGP-IgG, and IgA deficiency tests) and intestinal biopsies are the gold standard for diagnosing celiac disease and are prescribed by gastroenterologists. In addition to this, in some cases, genetic testing that confirms the existence of specific celiac disease-related genes (HLA-DQ2/HLA-DQ8) may be beneficial.
-
How accurate is a biopsy for celiac disease?
There are two methods of celiac disease biopsy, where a gastroenterologist can diagnose the condition.
- Skin biopsy: This is done if the patient has celiac disease associated with dermatitis herpetiformis (DH). It involves collecting small pieces of skin near the surroundings of a rash that occurred due to the presence of DH. The obtained sample is used to test for the presence of IgA antibodies.
- Intestinal biopsy: This test is the gold standard for diagnosing celiac disease. A scope will be introduced into the mouth, pass through the oesophagus and stomach, and reach the small intestine. It provides a clear view of the small intestine, and the gastroenterologist will collect small pieces of tissue. The tissue will be examined microscopically by a pathologist to search for indicators of celiac disease.
-
Can you have gluten intolerance without having celiac disease?
Yes, one can have gluten intolerance without having celiac disease. It is a condition called "non-celiac gluten sensitivity" (NCGS), with manifestations of gastrointestinal and extra-gastrointestinal symptoms in response to consuming gluten-containing foods. It differs from celiac disease, as the patient suffering from gluten intolerance or NCGS has no abnormal gene that causes autoimmunity.
-
Is celiac disease hard to diagnose?
Yes, a celiac disease might be hard to diagnose if the patient has symptoms similar to those of other intestinal problems such as inflammatory bowel disease (Crohn's disease and ulcerative colitis), intestinal infections, and an infected colon (diverticulitis), irritable bowel syndrome, etc. However, the patient’s medical and family history, blood, gene, and biopsy tests can aid in concluding the diagnosis of celiac disease.
-
Will a colonoscopy show celiac disease?
No, a colonoscopy might not be used to diagnose celiac disease, as it is used to examinethe areas of the large intestine, such as the rectum and colon. Celiac disease occurs in the small intestine region; therefore, using a colonoscopy cannot be justified in diagnosing celiac disease. However, if the patient suffers from symptoms originating from the large and small intestines, the gastroenterologist might prescribe a colonoscopy.
-
Does ANA test for celiac disease?
Yes, an antinuclear antibody (ANA) test may be used to diagnose celiac disease. It is a blood test used to detect the presence of ANA in the blood that will target and damage the nuclei of the body's own healthy cells (autoimmunity), leading to serious health conditions. In celiac disease, healthy small intestinal cells are damaged by the body's immune system through antibodies, leading to small intestine inflammation. Thus, the presence of ANA in the patient's blood sample may confirm the diagnosis of celiac disease.
-
Can celiac disease go away?
No, celiac disease cannot be cured immediately; however, its symptoms can be managed with supplements and anti-inflammatory agents, and the villi in the intestine can be recovered with a lifelong strict gluten-free diet. The symptoms will probably improve within a few days after abstaining from gluten-containing foods. In 3 to 6 months, the small intestine should fully recover; for elders, it might take two years to heal completely.
-
How contagious can celiac disease be?
Celiac disease is a serious autoimmune condition; it is not contagious. It occurs in genetically predisposed people and the ingestion of gluten results in damage to the small intestine. This condition is hereditary and runs in families. It can develop at any age after people start consuming gluten. If left untreated, it may lead to additional serious health problems.
-
Is celiac disease life threatening?
While celiac disease itself is not usually life-threatening, it may lead to severe complications, including malabsorption, malnutrition, lactose intolerance, and cancer (very rare). If a person has coeliac disease, it is recommended to avoid eating any gluten. Eating even tiny amounts of gluten may trigger symptoms of celiac disease and raise the risk of developing complications.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.

Our Locations
Subscribe to our newsletter and stay updated with the latest health information.
By clicking on subscribe now, you accept to receive communications from PACE Hospitals on email, SMS and Whatsapp.
Subscribe to PACE Hospitals News
Thank you for subscribing. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
-

Payment in advance for treatment (Pay in Indian Rupees)
For Bank Transfer:-
Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545
Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc)
Call us at 04048486868
ADDRESS
PACE Hospitals
Hitech City : Beside Avasa Hotel, Pillar No. 18, Hyderabad - 500081
Madinaguda: Mythri Nagar, Beside South India Shopping, Madinaguda, Hyderabad - 500050
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals as such.