Endometriosis Symptoms
Globally, about 25% of reproductive-age women suffer from chronic pelvic pain, one of the vital endometriosis symptoms. Early detection can help reduce the impact of endometriosis. This article thoroughly explores the symptoms, enabling better recognition and understanding of endometriosis. It will also discuss the causes and treatments for endometriosis.
What Is Endometriosis?
Endometriosis is a chronic disease that occurs when tissue similar to the lining of the uterus grows outside the uterine cavity in unwanted locations. This condition causes pelvic scarring and chronic inflammation. Moreover, endometriosis can lead to difficulty in getting pregnant.
Endometriosis is a common disorder affecting one in every ten girls and women of reproductive age globally. Consult your reproductive health provider if you experience:
- Pelvic pain that heightens during menstrual periods
- Severe period pain disrupting your daily life
- Constipation, diarrhoea, or the presence of traces of blood in poo or pee during menstruation
- Painful sex
- Trouble conceiving
- Painful pooping or peeing during menstruation
Early intervention can help diagnose endometriosis, prevent its advancement, and reduce the impact of the symptoms.
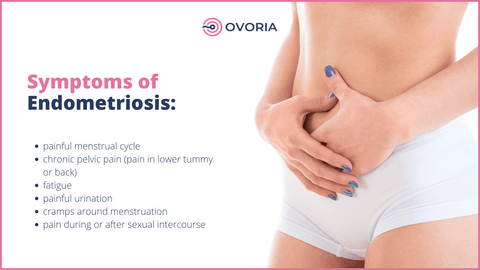
Endometriosis Symptoms
There are many symptoms of endometriosis, and the severity differs from one woman to another. Moreover, research revealed that the severity of the signs might not represent the seriousness of the disease. Let's take a detailed look at some common symptoms:
Pelvic Pain
One of the most common symptoms women with endometriosis experience is pelvic pain. The pain may persist past the periods and increase during sex, urination, or bowel movements. Analgesics and physical therapy can help reduce pain.
Painful Menstrual Cramps
Painful periods or dysmenorrhea are another most prevalent symptom of endometriosis. The pain may be frequent during, after, and even before your periods. Sometimes, it can be intense and spread out to your lower back through your legs, disrupting your daily life.
Pain During or After Intercourse
If you have endometriosis, you may experience severe pain during sex or afterward. Painful intercourse, or dyspareunia, results from endometrial tissue in locations like the bladder, ureter, bowel, fallopian tubes, and, in rare cases, the vagina.
Dyspareunia can rob you of your sexual intimacy and hurt your relationship. Open communication with your partner with the help and support of a fertility health specialist can help manage the symptoms and restore a healthy and happy sex life.
Heavy or Irregular Periods
All women have distinctive menstrual cycles; a typical situation for another woman might not be the case for you. Therefore, it may be difficult to tell when a particular symptom could mean something consequential.
Heavy periods are common but abnormal; it could indicate endometriosis or other gynaecological problems. You can tell you have an unusually heavy menstrual if:
- Tampons or pads soak quickly (within one hour or shorter)
- Bleeding goes on for more than a week
- You feel like vomiting or nausea
- You pass extensive blood clots
Women with endometriosis may also encounter spotting, post-period bleeding, or irregular periods. Non-period bleeding may be as heavy as actual menstrual periods. It can be helpful to have a gynaecological checkup when you experience these signs.
Pain With Bowel Movements
If the endometrial tissue develops in the rectum, intestines, bladder, or ureter, it can affect your urinary and bowel functions. As a result, you may experience bowel anomalies like bloating, constipation, diarrhoea, or blood in poo. And you could feel pain when pooping.
If the impact is on the urinary function, you may feel pain while urinating or an increased urination frequency. You should seek advice from your doctor if you notice anything unusual. They can help detect underlying conditions and offer a timely solution.
Bloating or Nausea
Fluid retention and bloating are common bowel symptoms of endometriosis. A study revealed that more women suffering from endometriosis experience abdominal bloating than those without. Endometriosis may lead to belly bloating for several reasons, including:
- Endometriosis can cause the formation of cysts with trapped blood in the ovaries, which may result in bloating.
- Women with endometriosis are susceptible to fibroids and small intestinal bacterial overgrowth (SIBO), which can cause bloating.
- Endometriosis tissue can cause inflammation and swelling in the abdomen, leading to bloating and water retention.
- Endometriosis usually causes digestive problems like constipation.
Infertility
Research shows that about 30% to 50% of women with endometriosis have infertility. Endometriosis can cause adhesion or scarring, which may block the fallopian tubes. As a result, the eggs will be unable to reach the womb, impairing your fertility.
Moreover, the inflammation caused by endometriosis may negatively impact implantation and egg quality. If you are struggling to get pregnant and suspect endometriosis, consulting your fertility healthcare provider can guide you on available treatment options.
Chronic Fatigue and Exhaustion
Sometimes, exhaustion and chronic fatigue can be a sign of endometriosis. Persistent pain, emotional stress, hormonal imbalances, and disrupted sleep due to discomfort can affect your well-being. Fatigue can have a significant impact on your daily life.
Overall, a multidisciplinary approach, including adequate rest, lifestyle changes, and emotional support, can help manage this condition.
Causes of Endometriosis
Although studies are ongoing to establish the exact cause of endometriosis, several factors are believed to contribute to its establishment. They include:
- Age: endometriosis can affect any woman or girl with menstrual periods. However, it is most prevalent among women in their 30s and 40s. However, there are treatments to help increase your chances of conception.
- Genetics: research has established that endometriosis runs in some families, meaning it could be a hereditary disease, and if your mother has endometriosis, for instance, you are likely to have it as well.
- Direct cell implantation: sometimes, endometrial cells attach to other areas, such as the abdominal wall, after a surgical procedure like a hysterectomy or a caesarean section. The cells may eventually develop and form lesions.
- Spread of cells: endometriosis may develop from endometrial stem cells spreading to other locations through the lymphatic system or blood.
- Reverse/retrograde menstruation: Endometrial tissue flows backward into the pelvic cavity during reverse menstruation. The tissue may get implanted and grow, causing endometriosis.
- Transformation of cells: other body cells outside the uterine cavity may transform into endometrial cells and grow into endometriosis tissue.
Treatments for Endometriosis
Endometriosis treatment aims to manage the symptoms and improve the quality of life. There are various treatment options available. Your doctor will help identify which option is suitable depending on the severity of symptoms and your preferences. Some of the treatment options include;
Pain Medication
Your physician may prescribe you anti-inflammatory pills to help relieve pain. They may recommend using a combination of pain relievers in case of severe pain.
Hormone Therapy
Hormone treatments aim at reducing or stopping oestrogen production—some work by inducing temporary menopause. Oestrogen promotes the growth and shedding of endometrial tissue. If your body stops producing this hormone, the endometriosis tissue will shrink or stop growing, reducing the pain.
However, hormone-based treatments cannot help with adhesions. Moreover, they reduce your chances of conception while on treatment, but this effect is not permanent. The primary hormone therapies for endometriosis treatment include:
Combined Oral Contraceptive Pill
This pill contains progesterone and oestrogen hormones. The medication works by suspending ovulation and making menstrual periods lighter. As a result, the periods are less painful if they occur.
Progestogens
Progestogens are artificial hormones that mimic the role of progesterone hormone to limit the growth of endometrium and endometriosis tissue. They include:
- The contraceptive implant
- The contraceptive injection
- The intrauterine system (IUS)
- Non-contraceptive progestogen tablets
- Progestogen-only-pill
Gonadotropin-releasing hormone (GnRH) Analogues
GnRH analogues induce temporary menopause by reducing oestrogen hormone production, helping stop the advancement of endometriosis. Your doctor may also prescribe them as post-surgery (laparoscopic surgery) therapy to help lessen pain.
Surgery
The physician may recommend a surgical procedure to eliminate endometriosis tissue and relieve the symptoms. Also, surgery can help with adhesions or scar tissue. It would help if you discussed with your doctor the risks and benefits of each surgical procedure and your fertility preferences, and they will help you decide which option suits you. Some surgery options for endometriosis treatment include:
Laparoscopy or Keyhole Surgery
Laparoscopy involves removing endometriosis tissue or adhesions using special surgical instruments through minute cuts (incisions) in the skin. The surgeon applies anaesthesia during the procedure, and you won't feel pain. Laparoscopy can help improve your chances of getting pregnant.
Hysterectomy
This more complex surgical procedure involves removing the uterus and sometimes the ovaries. This procedure is more effective as endometriosis is unlikely to recur if the surgeon removes the cervix and ovaries.
However, hysterectomy is irreversible, and you should consider it only if you don't plan to have children and other treatment options aren't successful.
Alternative Therapies
There are pain and stress management techniques that you can use as complementary therapies alongside other treatments. They include the following:
- Transcutaneous electrical nerve stimulator (TENS): The technique involves electrically stimulating the skin above the pain source points to relieve pain. This therapy helps manage chronic pelvic pain associated with endometriosis.
- Dietary changes: Research shows that adopting gluten-free diets rich in polyunsaturated fatty acids and low nickel can help lessen the pain attributed to endometriosis.
- Acupuncture therapy: some studies reported improved quality of life for endometriosis patients who use this therapy to manage pain.
Conclusion
Endometriosis is a condition that can significantly impact your day-to-day life and cause depression. Understanding endometriosis symptoms is crucial in reducing its impact. Some common signs of endometriosis include chronic pelvic pain, heavy or irregular periods, painful bowel movements, fatigue, and infertility. Treatment options available include hormone therapy, pain medication, and surgery. Moreover, lifestyle and dietary adjustments can help reduce the pain and impact of endometriosis. If you experience the symptoms outlined above, consult a reproductive endocrinologist. The physician can help identify a suitable treatment to improve your quality of life and chances of getting pregnant.
References
- FEDELE, L., BIANCHI, S., BOCCIOLONE, L., DI NOLA, G. I. U. L. I. A. N. A., & Parazzini, F. (1992). Pain symptoms associated with endometriosis. Obstetrics & Gynecology, 79(5), 767-769. Retrieved from https://journals.lww.com/greenjournal/abstract/1992/05000/pain_symptoms_associated_with_endometriosis.27.aspx
- Lemaire, G. S. (2004). More than just menstrual cramps: symptoms and uncertainty among women with endometriosis. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 33(1), 71-79. Retrieved from https://onlinelibrary.wiley.com/doi/abs/10.1177/0884217503261085
- Bulletti, C., Coccia, M. E., Battistoni, S., & Borini, A. (2010). Endometriosis and infertility. Journal of assisted reproduction and genetics, 27, 441-447. Retrieved from https://link.springer.com/article/10.1007/s10815-010-9436-1
Frequently Asked Questions
-
What Are Some Uncommon Symptoms of Endometriosis?
Some less common symptoms of endometriosis are increased urination frequency, back pain, difficulty breathing, and chest pain.
-
What Are the Symptoms of Severe Endometriosis?
Severe endometriosis symptoms include thick adhesions, substantial or enlarged ovarian cysts, and numerous deep implants.
-
What Are the Symptoms of Endometriosis After Menopause?
The symptoms of endometriosis in menopausal women include vaginal atrophy, hot flashes, night sweats, and mood swings.
Ovoria Egg Bank
Medicover Group
Antonovycha street, 102
79057 Lviv, Ukraine
info@ovoria.com
Privacy policy | Public offer | Cookies policy | Service Map | Ovoria Copyright 2024

