A Novel Surgical Technique Using Collagen-Based Artificial Dermis for Giant Omphalocele for which the Conventional Method was Ineffective: A Case Report
Received: 26-Apr-2021 / Accepted Date: 10-May-2021 / Published Date: 17-May-2021 DOI: 10.4172/2572-4983.1000215
Abstract
A Giant Omphalocele (GO) with marked viscero-abdominal disproportion is associated with surgical difficulty and higher morbidity and mortality rates. Despite various treatment strategies, no consensus exists on optimal GO management. We report our experience of a neonate with a GO that overcame the major therapeutic challenges (including formation of an incomplete silo, silo infection, and jejunal perforation) and succeeded in abdominal wall closure by introducing the novel idea of using Collagen-based Artificial Dermis (CAD) for epithelization. In conclusion, the treatment with CAD for epithelialization can be considered in cases where it is extremely difficult to return the viscera in conventional management.
Keywords: Giant omphalocele; Silo infection; Jejunal perforation; Negative pressure wound therapy.
Introduction
Omphalocele is one of the most common congenital abdominal wall defect with a birth prevalence of 1 per 4,000-6,000 livebirths, but a higher incidence if stillbirths and terminations of pregnancy are also taken into account. A Giant Omphalocele (GO) with marked visceroabdominal disproportion is associated with higher rates of morbidity and mortality, and it often represents a major surgical challenge. Although various treatment strategies such as primary repair, staged repair, and several delayed closures or non-surgical managements have been reported, there is no consensus on the optimal management for a GO [1].
We present our experience with a neonate with GO which showed a high degree of viscero-abdominal disproportion and complications such as difficulty in returning the liver due to adhesion between the hepatic vein and fascia, silo infection, and gastrointestinal perforation. We emphasize we overcame the complications and succeeded in closing the abdominal wall by epithelialization, utilizing a combination of previously reported Negative Pressure Wound Therapy (NPWT) [2] and collagen-based artificial dermis as a novel treatment method.
Presentation Of Case
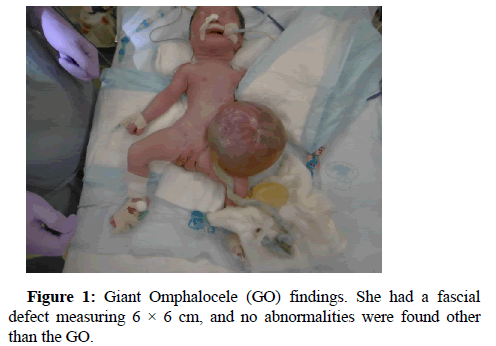
A Japanese female neonate was born at an estimated gestational age of 38 weeks with a birthweight of 3.047 kg, who had an intact GO with a fascial defect measuring 0.06 × 0.06 m (Figure 1). No other abnormalities were found on screening including postnatal echocardiography. As the sac was large, pedunculated, and unsupported, the sac rolled over.
The hemodynamics changed and became unstable, leading to low blood pressure. On the day of birth, a silo was formed using a small Size Wound Retractor (SWR) (Alexis Wound Retractor small size, Applied Medical Resources Corporation, Rancho Santa Margarita, CA, USA) to support the large sac. Since the hepatic veins were firmly adherent to the cranial end of the rectus fascia of the abdominal wall defect, the SWR could not be inserted through the fascial defect. Hence, the SWR was fixed to the abdominal wall. The incomplete silo resulted in poor repatriation of herniated viscera. In addition, the abdominal wall to which SWR was fixed was incised because numerous injuries had resulted from excessive tension that had been applied to fixed parts. Therefore, biomaterial (GORE-TEX® Soft tissue patch, W. L. Gore and Associates, Inc., Newark, NJ, USA) was sutured to each fascia to form a new silo after removing the SWR and sac. In addition, a sterile dressing of silver (AQUACEL® Ag Extra TM, ConvaTec, England and Wales) was attached to prevent infection in the silo. However, by day 51 the silo had become infected and resulted in bacteremia. The infected silo was removed quickly, but a large quantity of pus was noted adhering to the surface of the protruding viscera. A new silo was reformed using an SWR, and the infected surface was washed with saline daily.
Results
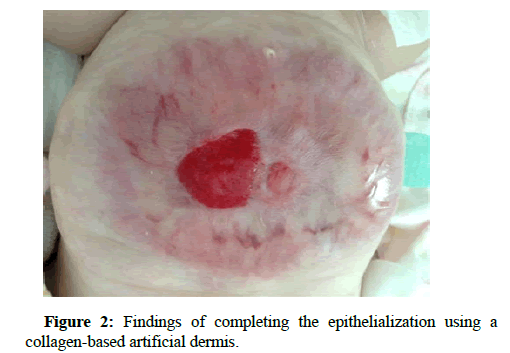
By day 65, the infection was under control. On the other hand, the abdominal wall had become thin and fragile. Hence, we decided that it would be impossible to close the wall by reducing the silo contents and considered the idea of epithelializing the abdominal wall defect, leading to closure. We applied artificial dermis onto the fibrous capsule and initiated epithelialization using NPWT. On day 71, Jejunal perforation was discovered when epithelialization progressed to about two-third of the total, after which the intestinal perforation became an intestinal fistula. On day 178, an incision was made along the intestinal fistula, and it was drawn out and repaired and a collagenbased artificial dermis was cut according to the size of the incision area and fixed by suturing. By day 247, epithelialization of the abdominal wall was almost complete (Figure 2), and on day 328, the patient was discharged from our hospital. She regularly visits our pediatric surgery outpatient department and was found to be well at the latest follow up.
Discussion
Although multiple management strategies have been developed for a GO, we failed to achieve abdominal wall closure with those conventional strategies in this case [1,3-5].
Bauman et al. [3] recommend that nonoperative delayed management be utilized as, Primary therapy for the newborn with a giant omphalocele because it has lower mortality rates and better clinical outcomes, but it has a higher incidence of sepsis, difficulty in wound care and needs correction of the ventral hernia later in life.
On the other hands, early closure of the abdominal wall is free of sac infections and can decrease hospital stay and time to full feeding, but can also lead to a sudden increase in intra-abdominal pressure and respiratory failure due to reduced lung capacity. Mustafa [6] reported the strategy of the combination of primary closure in the early period and conservative management of providing faster epithelialization with povidone-iodine and antibiotic powder together with elastic bandage application. This is an excellent strategy to not only make up for the weaknesses of non-operative management and primary closure, but also to take advantage of each. Here, since povidone-iodine has a risk for hypothyroidism, it seems useful to change to silver impregnated nanocrystalline dressing that systemic silver concentration are lower than silver sulfadiazine dressing [7,8] and Oquendo et al. [1] and Percy et al. [7] demonstrated no silver toxicities in their patients.
In our case, sac was pedunculated and easily twisted, so blood pressure could not be maintained without support, so these conventional treatments could not be applied and silo had to be constructed to support them.
Our patient presented with three major therapeutic challenges. One was the formation of an incomplete silo. In general, even with GO, if the silo can be properly attached, viscera can be repatriated intraperitoneally, but in this case, adhesion between the hepatic vein and fascia interfered with proper silo formation, and viscera repatriation did not proceed.
The second was silo infection. Although the silo made of biomaterial was fixed to the fascia and provided excellent support to the protuberant viscera, silo infection had led to the potential failure of viscera repatriation. The reports of successful viscera repatriation by silo formation using biomaterial were the cases without infection, and it seems that infection control is the key to the success or failure of this method.
The third was jejunal perforation. The infected prolapsed intestinal tract had a fragile intestinal wall even after the infection had been controlled, which was thought to be cause of the perforation during the process of epithelialization. In order to avoid this complication, it seemed important to prevent infection of prolapsed viscera.
The most important thing that this case succeeded in closing the abdominal wall was the change of treatment strategy from viscera repatriation to epithelialization of the abdominal wall using artificial dermis and utilizing the NPWT method.
Artificial dermis is a kind of tissue engineering dermal substitute and is used to repair dermal defects caused by a variety of reasons. When the artificial dermis is placed on skin defects, the pores of the inner collagen sponge are infiltrated by fibroblasts and capillaries. This cell-infiltrated membrane is gradually converted into a synthesized connective tissue matrix, similar to true dermis, as the original network of collagen sponge is biodegraded.
On the other hands, NPWT is one of the most successful mechanical adjuncts to wound healing. This modality may become an invaluable adjunct to wound management and other surgical applications.
We were able to achieve abdominal wall closure by introducing the novel idea of using the artificial dermis and NPWT to close the abdominal wall by epithelialization.
In addition, the defect with a diameter of 5 cm or more was found after intestinal fistula closure surgery in the abdominal wall formed by granules. It was impossible to primally suture and close the defect because the surrounding tissue was fragile. By filling the defect with the artificial dermis, suturing and fixing it, and then advancing epithelialization, it was possible to overcome such the large abdominal wall defect.
We believe that our experience can help in treatment choices in the future when similar complications are encountered.
Conclusion
Although two-stage surgery is required, treatment with collagenbased artificial dermis for epithelization can be considered in cases where it is extremely difficult to return the viscera to the abdomen or in cases where gastrointestinal perforation leads to difficulties in conventional management.
Funding
All authors declare that they have no funding source.
Author Contribution
Masaki Horiike (MH) made the conception and design of this Case Report. MH wrote the draft manuscript. All authors gave final approval of the version to be published. MH has overall responsibility and guarantees the scientific integrity.
References
- Oquendo M, Agrawal V, Reyna R, Patel HI, Emran MA, et al. (2015) Silver-impregnated hydrofiber dressing followed by delayed surgical closure for management of infants born with giant omphaloceles. J Pediatr Surg 50: 1668-1672.
- Aldridge B, Ladd AP, Kepple J, Wingle T, Ring C, et al. (2016) Negative pressure wound therapy for initial management of giant omphalocele. Am J Surg 211: 605-609.
- Bauman B, Stephens D, Gershone H, Bongiorno C, Osterholm E, et al (2016) Management of giant omphaloceles. A systematic review of methods of staged surgical vs. nonoperative delayed closure. J Pediatr Surg 51:1725–30.
- McNair aC, Hawes J, Urquaht H (2006) Caring for the newborn with an omphalocele. Neonat Netw 25: 319–27.
- Wagner JP, Cusick RA. Paint and wait management of giant omphaloceles. Semin Pediatr Surg 2019; 28: 95–100.
- Mustafa Erman Dörterler (2019) Management of Giant Omphalocele Leading to Early Fascial Closure. Cureus 11: e5932.
- Percy DB, Haddock C, Ma V, Nowak A, Panczuk J, Butterworth S (2018) Dressed for success? Silver impregnated nanocrystalline dressing for initial treatment of giant omphalocele. J Pediatr Surg 53:905-908.
- Malhotra A. Nanocrystalline silver dressing in the initial management of a giant omphalocele. J Paediatr Child Health 2010; 46: 365-366.
Citation: Horiike M, Kitada T, Santo K, Hashimoto T, Onishi S (2021) A Novel Surgical Technique Using Collagen-Based Artificial Dermis for Giant Omphalocele for which the Conventional Method was Ineffective: A Case Report. Neonat Pediatr Med 7:215. DOI: 10.4172/2572-4983.1000215
Copyright: © 2021 Horiike M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2154
- [From(publication date): 0-2021 - May 05, 2024]
- Breakdown by view type
- HTML page views: 1597
- PDF downloads: 557