How two newly approved gene therapies, including novel technology CRISPR, may help kids and adults with inherited blood disorders
9:30 AM
Author |

For children and adults with blood disorder sickle cell disease, the only curative treatment has long been a bone marrow transplant.
Now, the U.S. Food and Drug Administration has cleared the way for two groundbreaking gene therapies for the debilitating inherited disease – one of which is the first gene editing treatment to be used in humans.
University of Michigan Health teams have already begun work to address logistics involved with offering the therapies to patients ages 12 to 25 in the next year.
“We are actively engaged in advancing efforts within the field of pediatric hematology and bone marrow transplantation to introduce these revolutionary gene therapies,” said Ghada Abusin, M.D., a pediatric hematologist-oncologist and blood and marrow transplant specialist at U-M Health C.S. Mott Children’s Hospital.
“Clinical and research teams are dedicated to providing cutting edge solutions for individuals affected by sickle cell disease and other inherited disorders that affect red blood cells.”
Abusin, who is spearheading gene therapy initiatives for sickle cell disease at Michigan Medicine, answers questions about the new therapies below:
What is sickle cell disease?
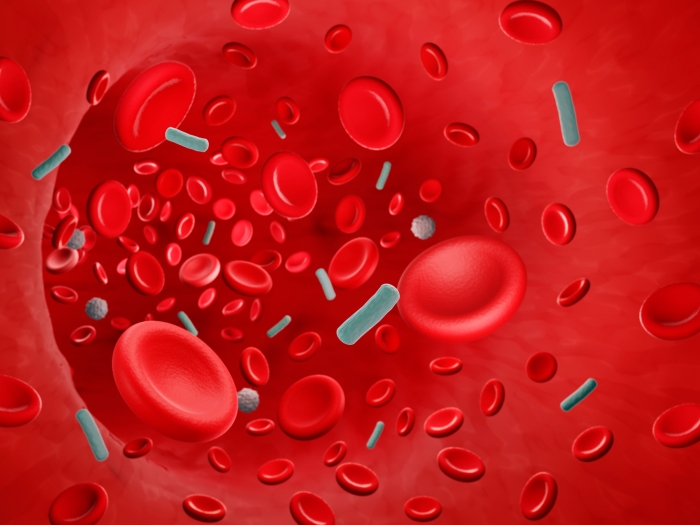
Sickle cell disease is a genetic condition that alters the shape of red blood cells from round and flexible to rigid and crescent shaped. This change can cause the cells to get stuck in small blood vessels, leading to blockages, pain, organ damage and a shortage of red blood cells, resulting in anemia.
Sickle cell disease is the most prevalent inherited blood disorder in the U.S., occurring when a child receives two sickle cell genes – one from each parent. It impacts roughly 100,000 Americans, including 3,500 Michigan residents, and millions worldwide.
While historically associated with people of African descent, sickle cell disease is diagnosed among various races and ethnic groups.
Individuals with the disease have a significantly shorter life expectancy, primarily due to early mortality during adulthood.
What are the differences between the two approved gene therapies?
Vertex Pharmaceutical’s Exa-cel, using the brand name Casgevy, is the first FDA-approved treatment to use the novel Nobel-Prize winning gene editing tool CRISPR. This therapy focuses on precisely manipulating the sequence of the existing human genome to manage diseases.
The FDA also approved a classical gene therapy for sickle cell called lovo-cel, made by the company bluebird bio and marketed as Lyfgenia. This conventional gene therapy involves adding new genes to human cells.
Lyfgenia, Abusin explains, gives patients a changed hemoglobin gene that can produce a new type of hemoglobin that has properties that help prevent sickling. The modified gene is added to the patients' own hematopoietic stem cells, which are early cells that develop into all types of blood cells in the body.
“The patient’s journey is similar for both therapies. They use different technologies to manipulate genes and return modified stem cells into patients,” Abusin said.
“These innovative gene therapies can potentially deliver more targeted and effective treatment for debilitating diseases like sickle cell that currently have limited therapy options.”
She emphasizes that neither tool is a 100% cure but are intended to be one time treatments to significantly alleviate pain and help prevent complications associated with the disease for a lifetime.
Meanwhile, U-M Health is also poised to soon offer Zynteglo, a gene therapy approved in 2022 for thalassemia, another inherited blood disorder that causes the body to have less hemoglobin than normal.
“We are actively engaged in advancing efforts within the field of pediatric hematology and bone marrow transplantation to introduce these revolutionary gene therapies.” - Ghada Abusin, M.D.
How do patients receive treatment?
Both gene therapies require a nearly yearlong process, starting with a series of blood transfusions that replace some sickled cells with healthy ones leading up to treatment.
Once sickle cells have been reduced to a low enough level, patients are hospitalized so doctors can extract their blood stem cells from their bone marrow, then their blood. Several extractions may be required to collect enough cells to be modified in the lab to make healthy hemoglobin.
Patients return three to six months later, once the genetically engineered (Casgevy or Lyfgenia) cells are ready and receive high dose chemotherapy to remove their existing bone marrow to receive the infusion of modified cells. They will likely stay at the hospital for another six to eight weeks, Abusin says.
“We will need to monitor them at the hospital to watch for infections and wait for healthy blood cells to show in their blood,” she said. “Families will be advised that undergoing this treatment can be a challenging and grueling process.”
Who is eligible?
Casgevy is approved for people ages 12 years and up with severe sickle cell disease and Lyfgenia is approved for those ages 12 to 50 years.
However, some conditions may prevent people from being eligible for the therapies, including a history of stroke or significant organ damage.
How do new therapies compare to current treatment for sickle cell?
A bone marrow, or stem cell, transplant is currently the only known cure for sickle cell disease. It also involves chemotherapy to eliminate and replace the abnormal stem cells in bone marrow with healthy cells from an eligible donor.
A bone marrow transplant may still be the recommended path for many people with severe sickle cell disease who have this option, Abusin says.
While transplants are often successful, some patients may experience serious complications, including infection, a failed transplant or graft versus host disease, in which donor bone marrow or stem cells attack the recipient.
Gene therapies, however, also come with risks, Abusin notes. Long term side effects are still unknown. Since both treatments require chemotherapy, patients may also experience side effects like lowered immunity and infection, infertility or potential for secondary cancer.
“These are exciting milestones, but every therapy has risks and benefits and these should be carefully evaluated for each specific patient,” Abusin said.
“It’s exciting to see advances in the field giving sickle cell patients new powerful tools and options to control this brutal disease and improve their quality of life.”
Other than a bone marrow transplant, hydroxyurea, L-glutamine, Voxelotor and Crizanlizumab aim to manage symptoms and reduce complications. Responses and outcomes, however, vary.
Will cost be a barrier?
Casgevy is priced at $2.2 million, while Lyfgenia has a higher cost of $3.1 million.
In the U.S., Abusin said, there are high hopes that Medicaid and Medicare will provide coverage to eligible Americans who are most likely to benefit from gene therapy.
Concerns about accessibility are particularly acute for other regions of the world where sickle cell is even more prevalent, particularly African nations, Abusin says.
“Sickle cell is a debilitating, painful and disruptive disease that shortens life expectancy,” Abusin said. “This is something that prevents people from leading a normal life. Things like exercise, getting too cold or being dehydrated can trigger a crisis episode.”
“We are optimistic that transformative treatments can reach those who need it most. But we know it will take a lot of time, work and advocacy to make it available to many.”
Because of the promise of technology like CRISPR, she adds, many in the field hope to see it become universally accessible.
“This is the first approved application of CRISPR, but this technology has potential to be used to treat various diseases in the future, including cancer, cystic fibrosis and many others,” Abusin said.
“This is the beginning of a new era in medicine.”

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!