Urology
Phimosis and Paraphimosis in Children
by
6th October 2023
10 minutes read
What is Phimosis in Children?
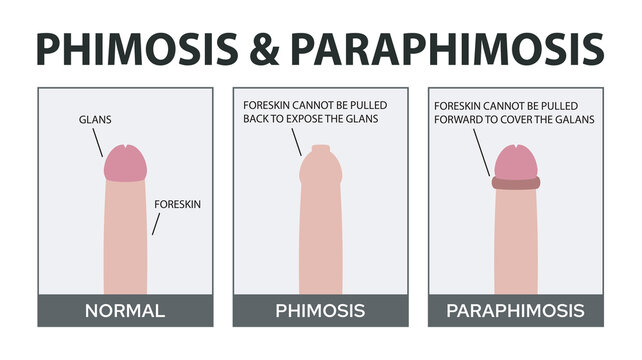
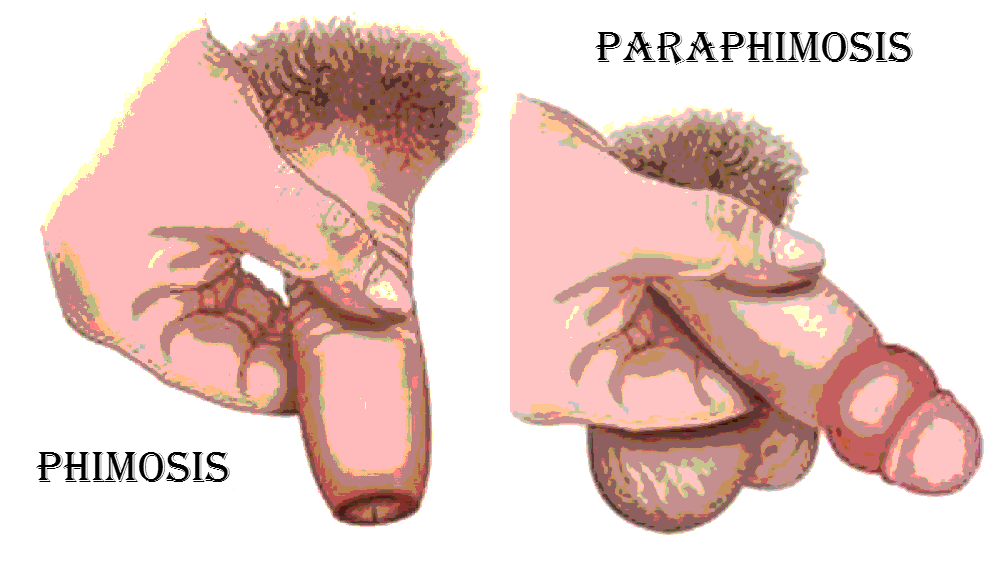
Phimosis refers to the inability to retract the foreskin (the skin covering the head, or glans, of the penis) due to its narrow opening. While phimosis is a normal physiological condition in newborn boys, it typically resolves on its own as a child grows. However, phimosis that persists beyond childhood or that presents with other symptoms may require medical attention.
Causes of Phimosis in Children:
1. Physiological Phimosis:
This is the most common type of phimosis in children. In newborn boys, the foreskin is often tight and stuck to the glans, making retraction difficult or impossible. As the child grows, the foreskin naturally becomes more pliable and separates from the glans. By the age of 3, approximately 90% of boys can retract their foreskin. By the age of puberty, about 99% can. Physiological phimosis is normal and doesn’t usually require treatment.
2. Pathological Phimosis:
This form of phimosis is due to scarring, inflammation, or infection. Causes include:
- Balanitis: Inflammation of the glans.
- Balanoposthitis: Inflammation of both the glans and the foreskin.
- Recurrent Infections: Multiple episodes can lead to scarring and tightening of the foreskin.
- Forceful Retraction: Forcibly trying to retract the foreskin before it’s ready can cause small tears, leading to scarring and subsequent tightening.
- Lichen Sclerosis (LS): A skin condition that affects the genital area, causing whitening and inflammation, and may lead to scarring.
3. Congenital Issues:
In some rare cases, children might be born with abnormal foreskin development, which can lead to phimosis.
Symptoms of Phimosis in Children
Phimosis in children refers to the condition where the foreskin cannot be fully retracted over the head (glans) of the penis. While it’s important to note that many young boys naturally have a non-retractable foreskin and this is normal, some children may develop symptoms that are indicative of a problematic phimosis. Here are some symptoms associated with phimosis:
- Swelling: The tip of the penis might appear swollen, especially if there’s an attempt to retract the foreskin.
- Pain and Discomfort: The child may complain of pain or significant discomfort in the penile region.
- Difficulty Urinating: In severe cases, the constriction and swelling might make it hard for the child to urinate, or there may be a weak urinary stream.
- Redness: The tip or the entire foreskin might become red and inflamed.
- Scarring: In cases of pathological phimosis, there might be visible white, ring-like scars at the tip of the foreskin.
- Discharge: There might be a foul-smelling discharge (smegma) under the foreskin.
Diagnosis and Treatment of Phimosis in Children
Diagnosing and treating phimosis in children involves understanding the nature of the phimosis (physiological versus pathological) and considering the child’s age, symptoms, and the severity of the condition.
Diagnosis:
- Physical Examination: A pediatrician or pediatric urologist will typically begin with a visual examination of the penis to determine the degree of phimosis and check for signs of inflammation or scarring.
- Medical History: The doctor will ask about symptoms, any previous attempts at foreskin retraction, a history of urinary tract infections, any previous treatments, and other relevant details.
- Urinalysis: If there’s a suspicion of infection or if the child has urinary symptoms, a urinalysis might be performed.
- Other tests: In rare cases, additional tests might rule out other conditions or confirm a specific diagnosis (like a biopsy for suspected lichen sclerosis, although this is uncommon).
Treatment:
- Observation: For physiological phimosis in younger children, often no treatment is necessary. The condition will likely improve on its own as the child grows.
- Topical Steroids: If the phimosis is thought to be amenable to non-surgical treatment, a doctor may prescribe a topical steroid cream. The cream is applied to the tip of the foreskin for a specified duration (usually a few weeks). This can help soften and stretch the foreskin and often resolves mild cases of phimosis.
- Manual Stretching: Sometimes, alongside the use of steroid creams, gentle manual stretching of the foreskin is advised. This should be done carefully, following a doctor’s instructions, to avoid causing tears or pain.
- Hygiene Guidance: Maintaining good penile hygiene can prevent infections and may help improve mild symptoms.
- Other Surgical Procedures: Depending on the exact issue and the anatomy of the child’s penis, other procedures, such as dorsal slit, might be recommended.
What is Paraphimosis in Children?
Paraphimosis is a urological emergency where the retracted foreskin cannot be returned to its original position, leading to constriction of the glans penis. This constriction can impair blood flow, potentially leading to swelling and damage to the penis. It’s important to distinguish between phimosis (where the foreskin cannot be retracted over the glans) and paraphimosis (where the retracted foreskin cannot be returned forward).
Causes of Paraphimosis in Children:
- Forceful Retraction: One of the most common causes in children is the forceful retraction of the foreskin, either by the child himself, a caregiver, or sometimes during medical examinations or procedures.
- Medical Procedures: Sometimes, after medical examinations or procedures like catheter insertion where the foreskin is retracted, it might not be returned to its original position, leading to paraphimosis.
- Vigorous Cleaning: Overzealous cleaning under the foreskin without returning it to its normal position can lead to paraphimosis.
- Swelling or Inflammation: Any condition that causes the tip of the penis to swell can make it difficult for the foreskin to return to its original position.
- Chronic Balanitis: Inflammation of the glans penis can lead to edema and difficulty in returning the foreskin to its normal position.
Symptoms of Paraphimosis in Children
Paraphimosis is a condition in which the foreskin, once retracted behind the glans penis, cannot be moved back to its original, forward position. The foreskin acts as a constricting band, potentially impairing blood flow to the glans. In children, recognizing the symptoms early is crucial as paraphimosis is considered a urological emergency.
Symptoms:
- Swollen Glans: The head of the penis appears swollen and may change color due to impaired blood flow. It can become dark red or bluish.
- Constricting Band: A tight, constricting band of the foreskin can be seen behind the head of the penis.
- Pain: The child may experience pain or discomfort.
- Difficulty Urinating: In severe cases, the swelling might impede the flow of urine.
- Change in Color: Due to restricted blood flow, the glans may change color. It can appear dark red, purplish, or even bluish, indicating a lack of oxygenated blood reaching the tissue.
- Tenderness to Touch: The affected area may be sensitive or tender when touched or examined.
Diagnosis and Treatment of Paraphimosis in Children
Paraphimosis is a urological emergency. Early diagnosis and prompt treatment are essential to prevent complications.
Diagnosis:
The diagnosis of paraphimosis is primarily clinical, based on physical examination and history.
- Physical Examination: The most apparent findings are the constricting band of the foreskin behind the glans and the swollen, possibly discolored glans.
- Medical History: Understanding the events leading up to the presentation can aid in diagnosis. Questions might revolve around recent catheterization, forceful foreskin retraction, or other medical procedures.
Treatment:
Immediate reduction of the paraphimosis is the goal. The steps and methods can vary, but generally include:
1. Manual Reduction:
This is the first-line treatment.
- Compression: Gentle, steady pressure is applied to the swollen glans using sterile gauze to help express the edema and trapped fluids.
- Foreskin Repositioning: While maintaining compression, the foreskin is gently manipulated back to its normal position over the glans.
2. Osmotic Method:
Granulated sugar or hypertonic saline-soaked gauzes are sometimes placed on the swollen glans. The osmotic effect helps draw out the fluid, reducing the swelling and potentially making manual reduction easier.
3. Puncture Technique:
In cases where other methods don’t work, a doctor might use a small needle to puncture the edematous foreskin in multiple spots, releasing the trapped fluid and facilitating the manual reduction of the foreskin. This method requires local anesthesia.
4. Surgical Intervention:
In rare cases, if the above methods fail or if there’s significant tissue damage, surgical intervention might be necessary. This could involve making a small incision in the constricting band of the foreskin to relieve the pressure. Circumcision might be recommended in recurrent cases or if there’s significant tissue injury.
5. Pain Management:
Analgesics or local anesthesia might be used to manage pain during the reduction process.
Preventive Measures for Phimosis & Paraphimosis
Preventing phimosis and paraphimosis involves understanding the natural development of the foreskin and adopting practices that reduce the risk of trauma, inflammation, and scarring. Here are some preventive measures:
For Phimosis:
- Avoid Forceful Retraction: Especially in infants and younger children, the foreskin is naturally fused to the glans, and it’s normal for it not to retract. Never try to force it back, as this can cause pain, tears, bleeding, and later, scarring.
- Good Hygiene: Teach older boys how to gently clean beneath the foreskin without forcibly retracting it. Regular cleaning can prevent the buildup of smegma, reducing the risk of infections and posthitis (inflammation of the foreskin).
- Recognize and Treat Infections Early: Conditions like balanitis can cause or exacerbate phimosis. Recognizing and treating infections promptly can prevent complications that lead to phimosis.
For Paraphimosis:
- Always Return the Foreskin: If the foreskin is retracted for any reason, like cleaning or a medical examination, always ensure it’s returned to its natural position covering the glans. This simple step can prevent paraphimosis.
- Educate Caregivers and Medical Staff: Parents, caregivers, and even medical professionals should be educated about the risks of leaving the foreskin in a retracted position, especially after procedures like catheter insertion.
- Avoid Unnecessary Retraction: Only retract the foreskin when necessary, such as during cleaning or specific medical examinations. Avoid excessive or forceful retraction.
- Prompt Treatment of Swelling or Inflammation: If there’s any swelling or inflammation of the glans or foreskin, seek medical advice promptly. Addressing these issues early can prevent the development of paraphimosis.
Conclusion
Phimosis and paraphimosis are conditions related to the foreskin in males. To prevent them, it’s vital to understand the natural development of the foreskin and avoid forceful retraction. Maintaining good penile hygiene, educating caregivers and medical professionals, and ensuring the foreskin is always returned to its natural position after retraction are key. Early detection and appropriate management reduce complications, ensuring the well-being of the child. Regular pediatric check-ups are essential for addressing concerns.
FAQs
While it varies, many boys will have a fully retractable foreskin by the age of 7. However, some might not have full retractability until adolescence. Each child’s development is different.
Phimosis refers to the inability to retract the foreskin over the glans. While a “tight foreskin” can be an informal way of describing this, phimosis is the medical term.
As with any surgical procedure, there are risks like infection, bleeding, and scarring. It’s essential to discuss these risks with a urologist or pediatric surgeon.
Yes. Balanitis, an inflammation of the glans, can lead to scarring and tightening of the foreskin, causing phimosis.
Yes, it’s common for the foreskin to be adhered to the glans in infants and young children. These adhesions typically break down naturally over time.
CATEGORIES
- ACL Reconstruction
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Gynecomastia
- Health
- Health Insurance
- Hernia
- hindi
- Hip Arthoscopy
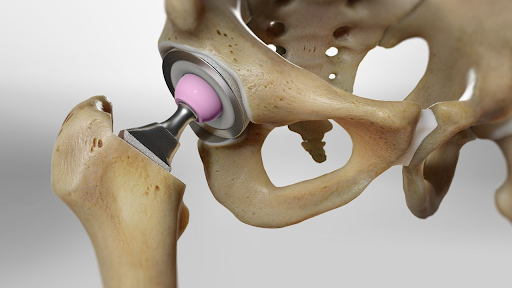
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Uncategorised
- Urology
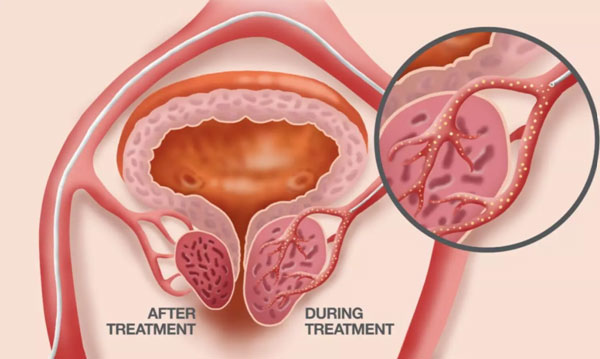
- uterine artery embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS