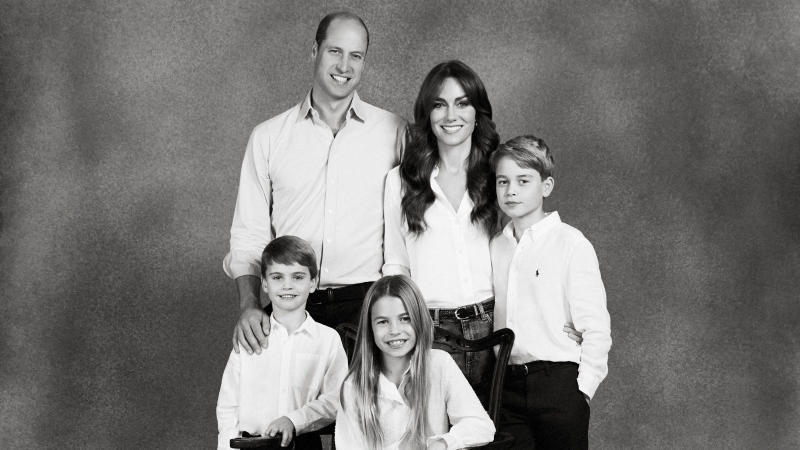
Prince William and Kate release photo of daughter Charlotte to mark ninth birthday
Prince William and his wife Kate released a picture of their daughter Charlotte to mark the princess's ninth birthday on Thursday.
In an unusual case study, a woman developed a black and hairy tongue after cancer treatment.
The rare phenomenon was described in a new paper published in the peer-reviewed journal BMJ Case Reports last month.
Doctors were first alerted to the issue when a woman in her 60s presented to a health-care facility for the treatment of hepatitis B. While doctors were assessing her, they noticed that she had grey, mottled patches on her skin that had not been there when she previously was at the facility three months earlier.
Upon further examination, they discovered that she had a patch of black pigmentation covering much of her tongue, and the bumps on her tongue had become prominent and hair-like.
Her tongue didn’t just look different than usual — it was painful as well, she told doctors.
A photo of the reaction shows a woman with a grey cast to her skin sticking out her tongue to show that it had changed colour, with darkness spreading out from the centre of her tongue like a stain.
She was diagnosed with black hairy tongue (BHT), which is a rare but reversible condition in which the tongue bumps (papillae) elongate and there is discolouration on the surface of the tongue.
The cause? A recent change in her cancer medication, according to the case report.
The woman has a 14 month history of post-operative chemotherapy for cancer with liver metastases, the report said, which had been undergone at a different hospital. But in the last four months, her chemotherapy was switched to new medications: panitumumab with irinotecan and 5-fluorouracil.
Although these are common medications associated with cancer and chemotherapy, the woman was also prescribed 100mg/day of minocycline to prevent skin lesions that can be caused by panitumumab.
At first, doctors were uncertain what the source was, as it could have been either the minocycline or the panitumumab that caused her BHT and hyper-pigmentation.
Both have been linked to BHT before, although the link between antibiotics such as minocycline is clearer. The facial hyper-pigmentation separate from the BHT led doctors to lean more towards minocycline, as it can lead to skin discolouration, with a 3-15 per cent incidence rate as a side effect.
She was immediately taken off of minocycline, and was given trifluridine and tipiracil hydrochloride plus bevacizumab combination therapy instead.
Her pigmentation and BHT had cleared up significantly at a check-in six weeks later, with the skin returned to a healthier tone and only a slight darkness remaining at the centre of the tongue.
According to the Mayo Clinic, BHT is a temporary and usually harmless oral condition in which the tongue takes on a “dark, furry appearance.” Part of the problem is a buildup of dead skin cells on the papillae, which can trap bacteria which exacerbates the discolouration. Possible causes include changes in the normal oral bacteria after antibiotic use, but BHT can also be caused by poor oral hygiene, overuse of mouthwashes with irritants such as peroxide, tobacco use and even eating too many soft foods that don’t allow dead skin cells to be sloughed off of the tongue due to friction.
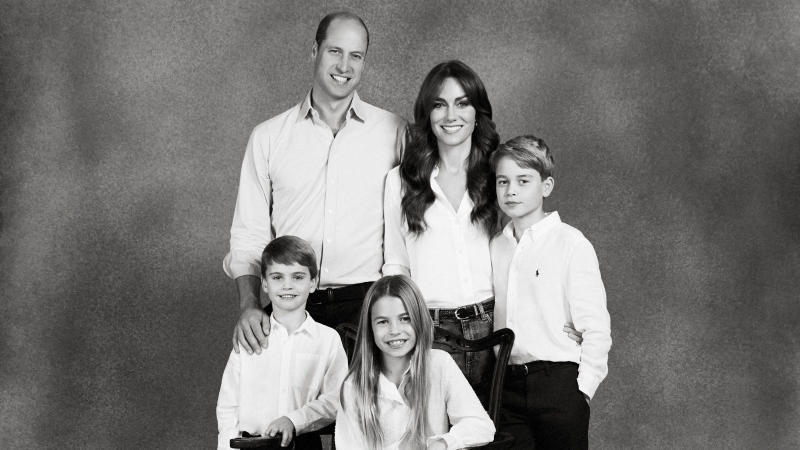
Prince William and his wife Kate released a picture of their daughter Charlotte to mark the princess's ninth birthday on Thursday.
The trusted traveller program between Canada and the United States is extremely popular and almost two million Canadians have a Nexus card.
Scientists studying a Neanderthal woman's remains have painstakingly pieced together her skull from 200 bone fragments to understand what she may have looked like.
One of the demands of pro-Palestinian activists who have set up protest encampments on university campuses in Canada and the United States is a severing of ties with Israeli universities.
Inspections are underway at more than one Loblaws location in Ottawa after complaints were filed about tall Plexiglas barriers.
The makers of Ozempic say their weight-loss drug Wegovy will be available to patients in Canada starting Monday.
Archeologists have unearthed the skeletons of five people, missing their hands and feet, at a former Nazi military base in Poland.
A Canadian restaurant lowered its prices this week, and though news of price tags dropping rather than climbing sounds unusual, the business strategy in this case is not, according to experts in the field.
In an effort to balance the profitability of Mother's Day with the pain it causes some people, some brands are offering customers the choice to opt out of Mother's Day email advertising.

A group of SaskPower workers recently received special recognition at the legislature – for their efforts in repairing one of Saskatchewan's largest power plants after it was knocked offline for months following a serious flood last summer.
A police officer on Montreal's South Shore anonymously donated a kidney that wound up drastically changing the life of a schoolteacher living on dialysis.
Since 1932, Montreal's Henri Henri has been filled to the brim with every possible kind of hat, from newsboy caps to feathered fedoras.
Police in Oak Bay, B.C., had to close a stretch of road Sunday to help an elephant seal named Emerson get safely back into the water.
Out of more than 9,000 entries from over 2,000 breweries in 50 countries, a handful of B.C. brews landed on the podium at the World Beer Cup this week.
Raneem, 10, lives with a neurological condition and liver disease and needs Cholbam, a medication, for a longer and healthier life.
The lawyer for a residential school survivor leading a proposed class-action defamation lawsuit against the Catholic Church over residential schools says the court action is a last resort.
Mounties in Nanaimo, B.C., say two late-night revellers are lucky their allegedly drunken antics weren't reported to police after security cameras captured the men trying to steal a heavy sign from a downtown business.
A property tax bill is perplexing a small townhouse community in Fergus, Ont.
 Diffuse grey pigmentation of the face and tongue covered with brownish-black patches is shown in this photo. (BMJ Case Reports)
Diffuse grey pigmentation of the face and tongue covered with brownish-black patches is shown in this photo. (BMJ Case Reports)