- Department of Neurosurgery, Hadassah University Medical Center, Jerusalem, Israel.
Correspondence Address:
Uri Pinchas Hadelsberg, Department of Neurosurgery, Hadassah University Medical Center, Jerusalem, Israel.
DOI:10.25259/SNI_743_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Uri Pinchas Hadelsberg, Lea Kahanov, Andres Vargas. Cerebellar liponeurocytoma with an unusual metastatic CSF spinal seeding. 11-Feb-2022;13:45
How to cite this URL: Uri Pinchas Hadelsberg, Lea Kahanov, Andres Vargas. Cerebellar liponeurocytoma with an unusual metastatic CSF spinal seeding. 11-Feb-2022;13:45. Available from: https://surgicalneurologyint.com/surgicalint-articles/11385/
Abstract
Background: Cerebellar liponeurocytoma is rare intracranial tumor appearing mostly in the posterior fossa.
Case description: We hereby report a long follow-up of a case of cerebellar liponeurocytoma in a 60-year-old female. At first, she presented in March of 2010 with the symptoms of hydrocephalus and was found to have a lesion located in the fourth ventricle. The tumor was resected with a small remnant around the brainstem which grew on serial imaging. Due to slow tumor growth, the patient was treated with conformal radiotherapy and was kept under follow-up with both outpatient visits and serial brain imaging. In 2018, due to low back pain and lumbar radicular pain, a new set of images of the spine was obtained which revealed multilevel intradural tumor spinal dissemination. The patient further underwent an open spinal biopsy at the level of L5 which revealed the same pathology of the intracranial tumor. The patient went on to receive total spine irradiation.
Conclusion: This case report describes a rare metastatic phenomenon to the spinal cord of the exact same pathology and grade of an intracranial cerebellar liponeurocytoma tumor.
Keywords: Cerebellar liponeurocytoma, CSF metastasis, Radiation
INTRODUCTION
Cerebellar liponeurocytoma is a relatively rare intracranial entity. Despite there being approximately 70 cases described in the medical literature of cerebellar liponeurocytomas and despite the pathology defined as a World Health Organization (WHO) Grade II tumor with a favorable prognosis, its natural history is not completely understood. Our case report describes an unusual characteristic of tumor aggressiveness hitherto unknown, showing its potential characteristic of leptomeningeal tumor dissemination, even without the development of malignant transformation per pathology report.
CASE PRESENTATION
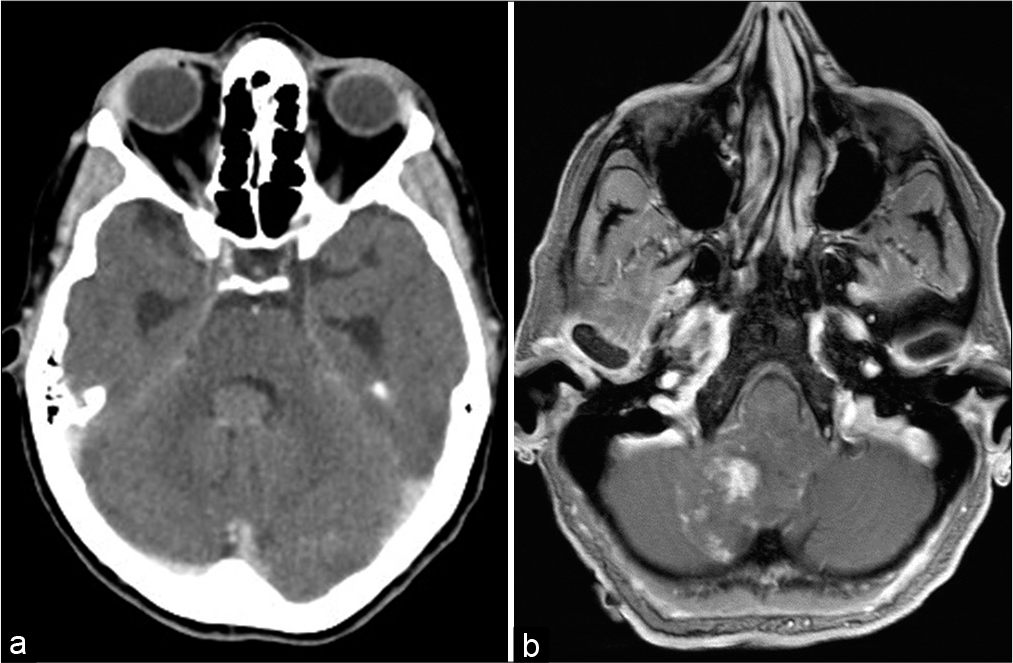
We present a case of a cerebellar liponeurocytoma which initially presented in a 61-year-old healthy female. The patient was admitted to the neurosurgical ward in March of 2010. At that time, the patient was admitted to the ER with a month long of general weakness and deterioration. On the day of admission, she complained of dizziness and urge incontinence. The patient’s physical examination was noticeable for a slight 4+5/5 right hand weakness and general weakness in her lower limbs as well as narrow-based walking. The patient underwent an initial CT scan and MRI [
The patient was followed up with serial MRI imaging being performed every 6 months. Due to new leg pain presented during follow-up, the patient underwent an FDG-PET in October 2017 scan to evaluate tumor metastases which demonstrated tumor spread to the cervical spinal canal. This prompted a total spine MRI [
In March 2021, the patient was seen during follow-up with stable disease both in her spine and her brain. Visual deterioration stopped after radiosurgery treatment. At present, the patient is at home with stable disease and no new neurological deterioration.
DISCUSSION
Regarding the pathology itself of a cerebellar liponeurocytoma, it was initially described as a WHO Grade I tumor. However, due to its substantial recurrences, the WHO assigned it a higher grade.[
In the pathology report, it was noted that the tumor had fragments of a neuroectodermal tumor with reactive gliosis with ill-defined neuronal rosettes and pseudorosettes. On immunostaining, the tumor stained positive for INI-1, S-100, GFAP, and vimentin, in accordance to the previous pathological reports of this tumor.[
In the most comprehensive review regarding these tumors, Oudrhiri et al. have noticed that only a bit more than 30 cases of this pathology were ever reported.[
This patient received radiation to the residual tumor in the brainstem. Residual tumor left after surgery is a feasible radiosurgery target and is a practice advocated by some authors.[
CONCLUSION
Much about this type of tumor remains unknown; however, some have already suggested that a high MIB-1 index and incomplete tumor resection might represent adverse prognostic factors in patients with liponeurocytoma.[
Our take-home message from this case is the potential feature of seeding metastasis in cerebellar liponeurocytomas and emphasizing that total tumor resection is superior in outcome compared to subtotal resection. Radiotherapy should be offered to patients, especially in the event of a subtotal resection.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bechtel JT, Patton JM, Takei Y. Mixed mesenchymal and neuroectodermal tumor of the cerebellum. Acta Neuropathol. 1978. 41: 261-3
2. Brat DJ, Parisi JE, Kleinschmidt-DeMasters BK, Yachnis AT, Montine TJ.editors. Surgical neuropathology update: A review of changes introduced by the WHO classification of tumours of the central nervous system, 4th edition. Arch Pathol Lab Med. 2008. 132: 993-1007
3. Cacciola F, Conti R, Taddei GL, Buccolieor AM, di Lorenz N. Cerebellar liponeurocytoma. Case report with considerations on prognosis and management. Acta Neurochir (Wien). 2002. 144: 829-33
4. Gembruch O, Junker A, Ahmadipour Y, Sure U, Lemonas E. Cerebellar liponeurocytoma-a rare entity: A case report. J Med Case Rep. 2018. 12: 170
5. Gembruch O, Junker A, Monninghoff C, Ahmadipour Y, Oppong MD, Sure U. Liponeurocytoma: Systematic review of a rare entity. World Neurosurg. 2018. 120: 214-33
6. George DH, Scheithauer BW. Central liponeurocytoma. Am J Surg Pathol. 2001. 25: 1551-5
7. Hirono S, Gao Y, Matsutani T, Ikeda J, Yokoo H, Iwadate Y. Metabolic, immunohistochemical, and genetic profiling of a cerebellar liponeurocytoma with spinal dissemination: A case report and review of the literature. Brain Tumor Pathol. 2021. 38: 257-62
8. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007. 114: 97-109
9. Oudrhiri MY, Raouzi N, El Kacemi I, El Fatemi N, Gana R, Maaqili MR. Understanding cerebellar liponeurocytomas: Case report and literature review. Case Rep Neurol Med. 2014. 2014: 186826
10. Patel N, Fallah A, Provias J, Kha NK. Cerebellar liponeurocytoma. Can J Surg. 2009. 52: E117
11. Xu L, Du J, Wang J, Fang J, Liu Z, He Y. The clinicopathological features of liponeurocytoma. Brain Tumor Pathol. 2017. 34: 28-35