Pelvic Inflammatory Disease, PID - Endometritis, Salpingitis, Peritonitis, Etiological agents, Lab Diagnosis
Introduction to Pelvic Inflammatory Disease (PID)
Pelvic Inflammatory Disease (PID) is an infection that results when cervical micro-organisms travel upward to the endothelium (inner membrane of the uterus), fallopian tube, cervix, and ovaries. This infection can cause the following conditions (1 or more)
endometritis
salpingitis (inflammation of the fallopian tube)
localized or generalized peritonitis (inflammation of the abdomen’s lining- peritoneum)
abscess of the fallopian tube or ovaries
Patients with Pelvic Inflammatory Disease (PID) often have intermittent abdominal pain and tenderness, vaginal discharge, dysuria, and severe back pain. Systemic symptoms such as fever, weight loss, and headache may also occur.
If Pelvic Inflammatory Disease (PID) is left untreated, serious complications such as permanent scarring of fallopian tubes and infertility may occur. It is more common in sexually active women and in cases of pregnant women, it is fatal and may cause death, or miscarriage.
Neisseria gonorrhoeae and Chlamydia trachomatis are the major causative agent. Other organisms such as anaerobes, gram-negative rods, Streptococci spp., and Mycoplasma spp. may ascend through the cervix, particularly after parturition, dilation of the cervix, or abortion.
The presence of Intrauterine (IUD) is associated with a higher rate of Pelvic Inflammatory Disease (PID). In presence of IUD, Actinomyces spp. may also cause PID.
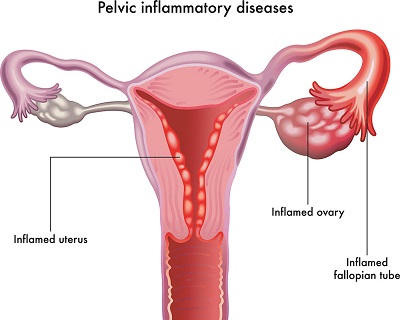
PID (Figure: Health direct)
Laboratory diagnosis of PID by Neisseria gonorrhoeae
Neisseria gonorrhoeae are gram-negative, intracellular kidney-shaped diplococci present between polymorphonuclear (PMN) leukocytes with few extra bacteria outside the cell. It inflames the urethra and progresses to cause Pelvic Inflammatory Disease (PID).
Sample
cervical swab
*Samples should be collected in such a way as to prevent vaginal flora contamination.
Intrauterine contents can be collected through an aspiration-protected suction curetting device or a double-lumen sampling device.
Microscopy
After microscopy, the presence of gram-negative, intracellular kidney-shaped diplococci lying between PMN with few extra bacteria outside the cell.
Culture
Etiological agents of Pelvic Inflammatory Disease (PID) can be cultured in artificial media.
Media used
Thayer Martin Agar with Vancomycin is not used as it inhibits 3-10% Neisseria gonorrhoea. Modified NYC media contains Lincolycin and are used as selective media.
Incubation at done at 37°C for 24 hours with 5-10% CO2.
Colony
* (observation and presumptive identification)
In modified NYC medium, a small raised greyish-white colony is observed
Biochemical test
The biochemical tests used for diagnosis of Pelvic Inflammatory Disease (PID) are:
Oxidase test: positive
take a cotton bud and dip it in oxidase reagent and ouch it to the colony
if the color changes to purple within 15 seconds, it may be Neisseria gonorrhoea.
Rapid Carbohydrate Utilization test
Glucose | Maltose | Lactose | Sucrose | |
|---|---|---|---|---|
Neisseria gonorrhoeae | + | + | - | - |
Neisseria meningitidis | + | - | - | - |
Coagglutination test
A suspension of Staphylococcus aureus coated with a specific antibody is treated with culture cells. If Neisseria gonorrhoeae is present, it gives an agglutination reaction which is known as coagulation.
Laboratory diagnosis of PID by Chlamydia trachomatis
The laboratory diagnosis of PID by Chlamydia trachomatis.
Sample
swabs, aspirates from the cervix, fallopian tube
Microscopy
For diagnosis of Chlamydia trachomatis, specimens are demonstrated by the presence of chlamydial inclusion bodies. The inclusion bodies are stained by Giemsa, Castaneda, macchiavello, or Gimenez for demonstration.
Culture
As Chlamydia trachomatis are intracellular, they can't be cultured in media. However, cell lines such as HeLa 229, Monkey Kidney cells, and McCoy (cyclohexidine treated) are the most commonly used.
Antigen detection
Antigen detection tests used for diagnosis of Chlamydia trachomatis include:
Direct fluorescent antibody (DFA)
EIA (enzyme Immuno Assay)
Cytologic examination
Cytologic examination of cell scrapings from the conjunctiva of newborns or persons with ocular trachoma detects inclusions after Giemsa stain. They are insensitive compared to other methods.
Serodiagnosis
Serodiagnosis of Chlamydia trachomatis are:
CFT (complement fixation test)
MIF (Microimmuno fluorescence)
ELISA
Molecular test
Molecular tests of Chlamydia trachomatis are:
Nucleic Acid Hybridization
SDA (strand displacement amplification)
TMA (transcription-mediated amplification)
PCR