Henry Suarez RDMS (AB, OB/GYN, PS) RVT
Phyllodes Tumor
Phyllodes tumors are uncommon breast lesions that consist of connective tissue and epithelium. The spectrum of behavior from phyllodes ranges from benign (comparable to fibroadenoma) to malignant with metastatic potential. Historically these lesions were called cystosarcoma phyllodes, though now are referred to as phyllodes due to their usual benign nature. [1]
Malignant Phyllodes tumor constitutes 20–30 % of all PTs of the breast. [15]
Epidemiology and Risk Factors
These tumors are usually rare and account for less than 1% of all breast neoplasms. [2]
The median age of phyllodes is 42-45 years but can be seen in females as young as 10 and as old as 82 respectively. [3] The older the patient, the likelier it is for the tumor to be a higher grade. Phyllodes tumor has been linked to Li-Fraumeni syndrome (an autosomal dominant inherited condition which leads to an increased risk in developing certain cancers). [4] There has also been a small association of phyllodes in patients with the BRCA1 gene and less so with BRCA2. [5]
Causes
The cause of phyllodes is unknown.
Radiological Appearance
Imaging findings are nonspecific to phyllodes and may appear like fibroadenomas. Most benign lesions present as firm, non palpable, lobulated masses with variable size averaging 5cm [1]
Mammography
Phyllodes may present as round densities with smooth borders radiologically indistinguishable from fibroadenomas. [1,6]
Ultrasound
Patients with suspicious or palpable masses are often referred to ultrasound for further evaluation. Phyllodes tumors can exhibit characteristics similar to fibroadenomas such as; hypoechoic, well demarcated, solid. Features like rapid growth, large size at presentation and cystic areas can raise suspicion for phyllodes.



Fig. 1-3 17 yo Female with complex cystic/solid breast lesion that resulted to be phyllodes.
Magnetic Resonance
Much like mammography and ultrasound, phyllodes can not be confidently distinguished from fibroadenomas on MRI. MRI has been used to help determine the extent of disease and potential resectability. [7] Calcifications are rare due to their rapid growth, however they have been reported. [7] MRI findings are typically of with a well-defined lobulated mass with a diameter ≥3 cm, isointense on T-1 weighted images and high signal on T2-weighted images.Other features are multi-nodule fusion appearance with internal hypointense septations. [7]
Diagnosis
Work up phyllodes tumors require a detailed physical and history along with imaging.
Percutaneous Procedures
Lesions that are deemed suspicious should be further worked up for tissue classification with fine needle aspiration or core biopsy. Of the two fine needle aspiration is less accurate in rendering a diagnosis.
Fine Needle Aspiration
Fine needle aspiration (FNA) is associated with a high false negative in the diagnosis of phyllodes. Cytologically phyllodes represent characteristics of epithelial and stromal tissues. The diagnostic parameters relate to the stroma with stromal nuclear atypia, isolated stromal cells with bare nuclei, and blood vessels crossing the stromal fragments.
Core Biopsy
Core biopsy has been under investigated in the diagnosis of phyllodes tumors. Microscopic features of phyllodes are elongated ductal and epithelium lined papillary projections of stromal tissue which produce the leaf-like appearance from which the tumor’s name is derived [8] (phyllodes is taken from the Greek language and means “leaflike”). Reportedly core biopsy has a false negative rate of about 25-30%. [9]
Gross Pathology
Upon gross examination and akin to radiological examination phyllodes can be indistinguishable from fibroadnomas. Characteristics of phyllodes are round to oval multinodular masses with a grayish-white appearance that are similar in appearance to cut cauliflower.
Treatment
Given the high incidence of recurrence complete surgical resection should be performed. Current guidelines recommend excisional biopsy for benign lesions, while for borderline and malignant lesions the entire mass should be surgically resected with at least 1 cm surgical margins. [10]
Mastectomy – Breast-Conserving vs. Total
In the case of adequate margins via resection and radiation therapy breast-conserving surgery has been found to be as effective as total mastectomy in treating malignant phyllodes. [11] Axillary dissection is typically not recommended due to the low (<1%) involvement of axillary lymph nodes. Mastectomy is not recommended for benign phyllodes except for in cases where the tumor is so large surgical excision will result in cosmetically undesirable results.
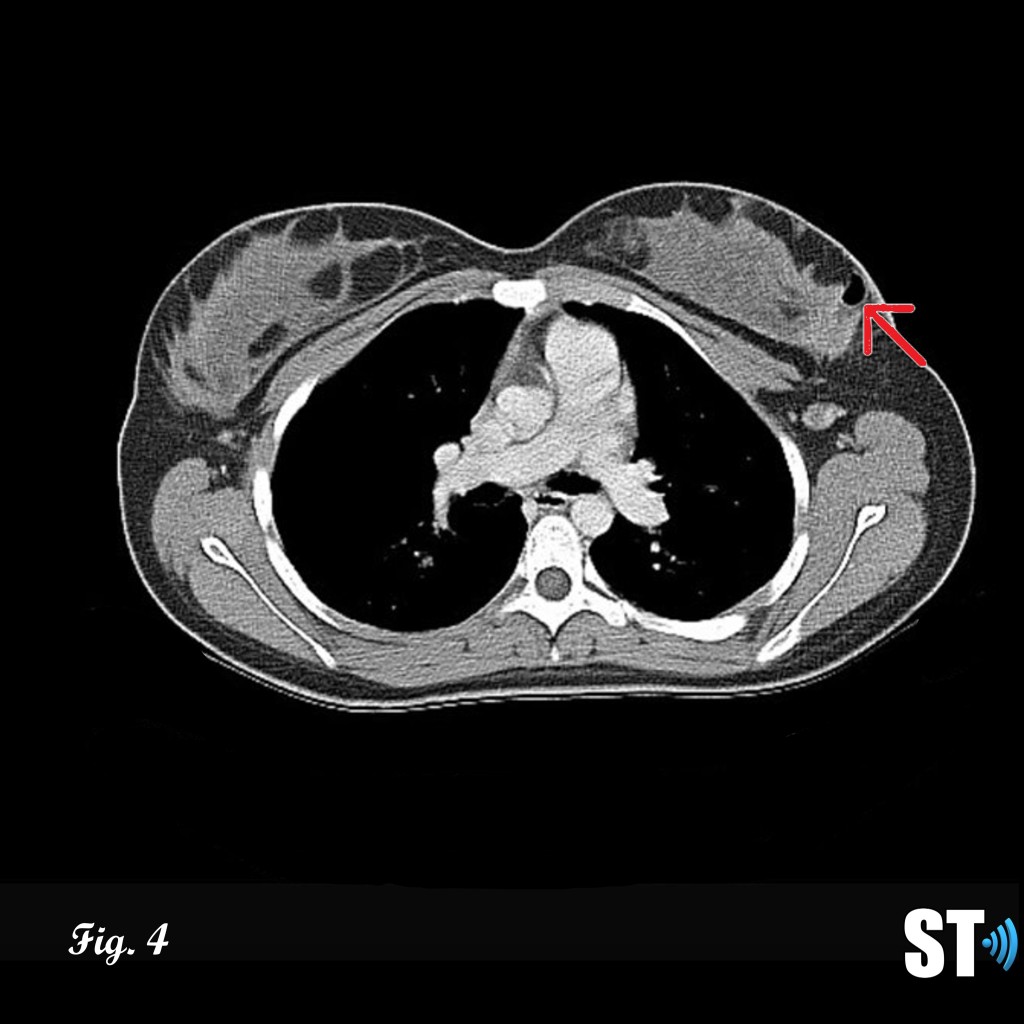

Figure 4-5 follow up post lumpectomy with post-surgical changes (air, red arrow) lesion was found to be malignant phyllodes resulting in mastectomy Fig.5 with breast implant in place (white asterisk).
Chemotherapy
Given the high incidence of recurrence chemotherapy is of questionable use and efficacy remains arguable. An observational study using Doxorubicin (a chemotherapy agent used commonly in the treatment of leukemia/Hodkin’s lymphoma) alongside Dacarbazine (commonly used in melanoma) failed to show no benefit in relapse free survival. [10]
Hormone Therapy
Currently hormone therapy has little to no value in treating malignant phyllodes. [10]
Prognosis
Phyllodes has been reported to have a recurrence rate of 10-25% for benign and borderline tumors [12] and up to 40% of all histological types. [13] Local recurrence [13] is more common than distant metastasis [14]. The prognostic implication deteriorates when metastasis is involved. Metastatic disease is quite aggressive, behaving like sarcomas, spread hematogenously and includes these common sites; lung, brain, abdominal viscera, bone and more rarely sites like duodenum, heart, parotid and oral cavity. [14] Metastasis is a poor prognostic factor with few patients surviving past 1 year. [16]
Conclusion
Phyllodes presents a difficult to diagnose lesion radiologically, with characteristics similar to fibroadenoma. It requires in depth investigation with Oncologists and tissue sampling to confidently arrive at the proper diagnosis. Phyllodes run the gamut from benign to malignancy and metastasis. Metastatic lesions offer a poor prognosis to the patient.
Bibliography
- V. Suzanne, and Kelly K Hunt. “Diseases of the Breast.” Sabiston Textbook of Surgery, 21st ed, Chapter 35., 809–55. Elsevier, 2022.
- Reinfuss M, Mituś J, Duda K, Stelmach A, Ryś J, Smolak K. The treatment and prognosis of patients with phyllodes tumor of the breast: an analysis of 170 cases. Cancer. 1996 Mar 1;77(5):910-6.
- Hanby, A.M., walker, C. Tavassoli FA, Devilee P: Pathology and Genetics: Tumours of the Breast and Female Genital Organs. WHO Classification of Tumours series – volume IV. Lyon, France: IARC Press. Breast Cancer Res 6, 133 (2004).
- Birch JM, Alston RD, McNally RJ, Evans DG, Kelsey AM, Harris M, Eden OB, Varley JM. Relative frequency and morphology of cancers in carriers of germline TP53 mutations. Oncogene. 2001 Aug 2;20(34):4621-8.
- Rosenberger, L.H., Thomas, S.M., Nimbkar, S.N. et al. Germline Genetic Mutations in a Multi-center Contemporary Cohort of 550 Phyllodes Tumors: An Opportunity for Expanded Multi-gene Panel Testing. Ann Surg Oncol 27, 3633–3640 (2020).
- Calhoun K, Allison KH, Kim JN, et al.. Phyllodes tumors. In: Diseases of the breast, Harris J, Lippman ME, Morrow M, Osborne KC (Eds), Lippincott Williams and Wilkins, 2014.
- Imaging findings in phyllodes tumors of the breast. AU Tan H, Zhang S, Liu H, Peng W, Li R, Gu Y, Wang X, Mao J, Shen X SO Eur J Radiol. 2012 Jan;81(1):e62-9. Epub 2011 Feb 25.
- Optimising preoperative diagnosis in phyllodes tumour of the breast. AU Jacklin RK, Ridgway PF, Ziprin P, Healy V, Hadjiminas D, Darzi A SO J Clin Pathol. 2006;59(5):454. Epub 2006 Feb 6.
- Needle core biopsy in the diagnosis of phyllodes neoplasm. AU Dillon MF, Quinn CM, McDermott EW, O’Doherty A, O’Higgins N, Hill AD SO Surgery. 2006;140(5):779.
- National Comprehensive Cancer Network (NCCN). NCCN Clinical practice guidelines in oncology (NCCN Guidelines). Phyllodes tumor. Version 1.2021. Available at: http://www.nccn.org (Accessed on February 21, 2021).
- Surgical treatment of borderline and malignant phyllodes tumors: the effect of the extent of resection and tumor characteristics on patient outcome. AU Onkendi EO, Jimenez RE, Spears GM, Harmsen WS, Ballman KV, Hieken TJ SO Ann Surg Oncol. 2014 Oct;21(10):3304-9. Epub 2014 Jul 18.
- Tan, BY, Acs, G, Apple, SK, Badve, S, Bleiweiss, IJ, Brogi, E, Calvo, JP, Dabbs, DJ, Ellis, IO, Eusebi, V, Farshid, G, Fox, SB, Ichihara, S, Lakhani, SR, Rakha, EA, Reis-Filho, JS, Richardson, AL, Sahin, A, Schmitt, FC, Schnitt, SJ, Siziopikou, KP, Soares, FA, Tse, GM, Vincent-Salomon, A & Tan, PH (2016) Histopathology 68, 5– 21. Phyllodes tumours of the breast: a consensus review
- Zhou ZR, Wang CC, Yang ZZ, Yu XL, Guo XM. Phyllodes tumors of the breast: diagnosis, treatment and prognostic factors related to recurrence. J Thorac Dis. 2016 Nov;8(11):3361-3368.
- Ramakant, P., Selvamani, Therese, M. M., & Paul, M. J. (2015). Metastatic Malignant Phyllodes Tumor of the Breast: An Aggressive Disease-Analysis of 7 Cases. Indian journal of surgical oncology, 6(4), 363–369.
- Ramakant P, Chakravarthy S, Cherian JA, Abraham DT, Paul MJ. Challenges in management of phyllodes tumors of the breast: a retrospective analysis of 150 patients. Indian J Cancer. 2013;50:345–348.

