Table of Contents
ToggleAddison’s disease
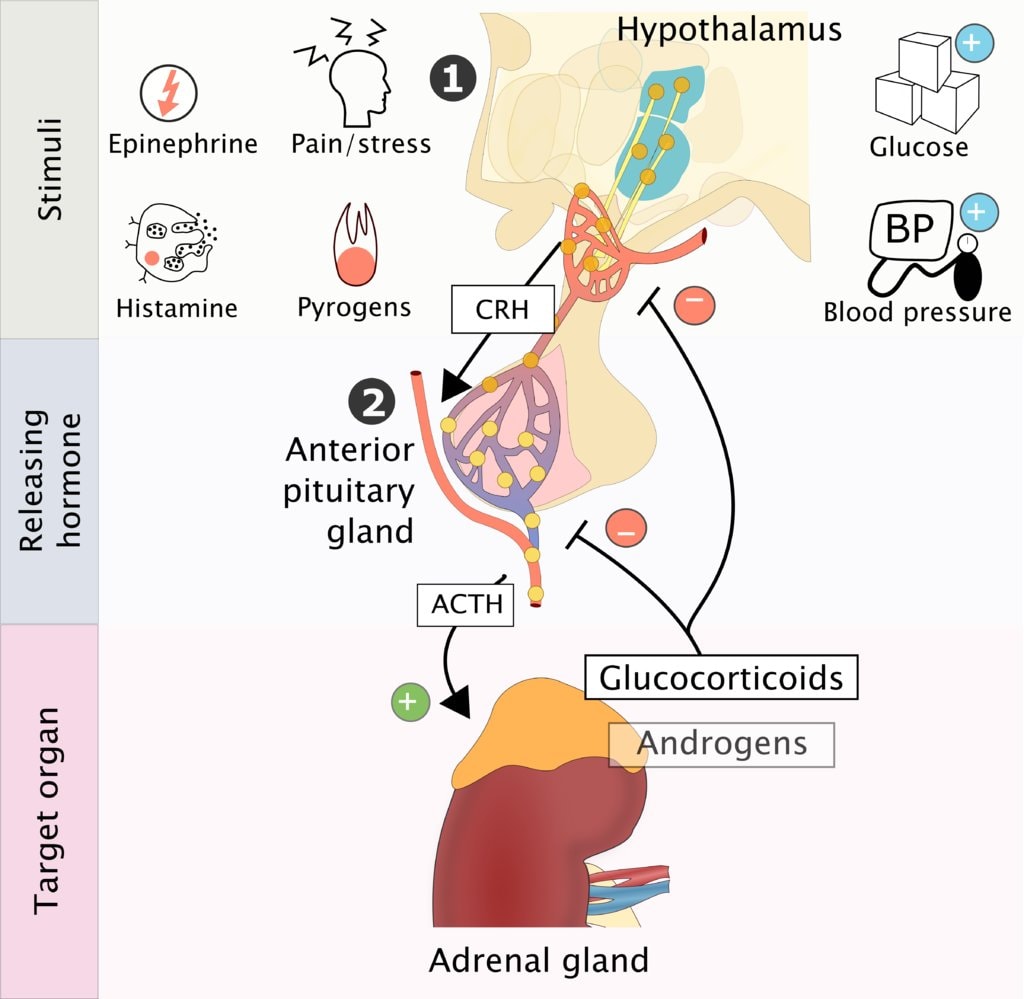
Addison’s disease is a clinical condition characterized by adrenocorticotrophic hormone hyposecretion due to primary disease of the adrenal glands or secondary to pituitary gland disorder.
It’s mostly idiopathic or auto immune but can occur in tuberculosis infection of the gland or obstruction by the adrenal tumor, metastasis / hemorrhage
Pathophysiology
- Adrenal glands are incapable of producing sufficient cortisol and other steroids . It is distinguished from acute primary adrenocortical insufficiency caused by Waterhouse-Friderichsen syndrome.
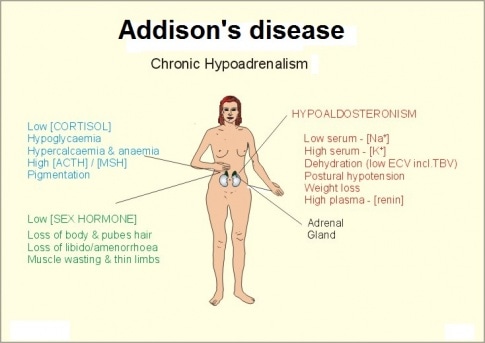
Mineralocorticoid deficiency: Because mineralocorticoids stimulate sodium reabsorption and potassium excretion, deficiency results in increased excretion of sodium and decreased excretion of potassium, chiefly in urine but also in sweat, saliva, and the gastrointestinal tract. A low serum concentration of sodium (hyponatremia) and a high concentration of potassium (hyperkalemia) result.
Urinary salt and water loss cause severe dehydration, plasma hypertonicity, acidosis, decreased circulatory volume, hypotension, and, eventually, circulatory collapse. However, when adrenal insufficiency is caused by inadequate adrenocorticotropic hormone (ACTH) production (secondary adrenal insufficiency), electrolyte levels are often normal or only mildly deranged, and the circulatory problems are less severe.
Glucocorticoid deficiency: Glucocorticoid deficiency contributes to hypotension and causes severe insulin sensitivity and disturbances in carbohydrate, fat, and protein metabolism. In the absence of cortisol, insufficient carbohydrate is formed from protein; hypoglycemia and decreased liver glycogen result. Weakness follows, due in part to deficient neuromuscular function. Resistance to infection, trauma, and other stress is decreased. Myocardial weakness and dehydration reduce cardiac output, and circulatory failure can occur.
Decreased blood cortisol results in increased pituitary ACTH production and increased blood beta-lipotropin, which has melanocyte-stimulating activity and, together with ACTH, causes the hyperpigmentation of skin and mucous membranes characteristic of Addison disease. Thus, adrenal insufficiency secondary to pituitary failure does not cause hyperpigmentation.
Causes of Addison’s Disease(Can be predisposing Factors too)
Autoimmune Reaction: Addison’s Disease can occur when the body’s immune system mistakenly attacks and damages the adrenal glands. This is known as an autoimmune reaction. In this case, the immune system views the adrenal glands as foreign entities and targets them for destruction, leading to a deficiency in adrenal hormones.
Idiopathic Atrophy of the Adrenal Glands: In some cases, the adrenal glands may undergo atrophy, which means they shrink and lose their function without a clear identifiable cause. This condition is referred to as idiopathic adrenal atrophy.
Surgical Removal of Both Adrenal Glands: Addison’s Disease can result from the surgical removal of both adrenal glands. This usually occurs as a last resort when treating conditions such as Cushing’s syndrome or adrenal tumors. After removal, the individual will need hormone replacement therapy.
Adrenal Carcinoma: Adrenal carcinoma is a rare type of cancer that originates in the adrenal glands. In some instances, the cancerous growth can disrupt the normal functioning of the adrenal glands, leading to adrenal insufficiency and Addison’s Disease.
Infections such as TB: Certain infections, particularly tuberculosis (TB), can infiltrate and damage the adrenal glands. TB-induced damage to the adrenal glands can impair their ability to produce hormones, causing Addison’s Disease.
Abnormal/Malfunction of the Pituitary Gland: The pituitary gland plays a crucial role in regulating adrenal function by secreting adrenocorticotropic hormone (ACTH). If the pituitary gland malfunctions and doesn’t produce an adequate amount of ACTH, the adrenal glands won’t receive the necessary signals to produce hormones, leading to Addison’s Disease.
Prolonged Use of Steroid Medication: Long-term use of corticosteroid medications, which are often prescribed for conditions like autoimmune diseases or inflammation, can suppress the production of ACTH by the pituitary gland. This can lead to adrenal gland atrophy and result in Addison’s Disease.
Additional causes include:
Genetic Factors: While most cases of Addison’s Disease are not inherited, there is a rare genetic form known as familial glucocorticoid deficiency (FGD). In FGD, specific genetic mutations can lead to the inadequate production of adrenal hormones.
Hemorrhage into the Adrenal Glands: Severe bleeding into the adrenal glands, often due to injury or other medical conditions, can damage the glands and impair their hormone production.
Amyloidosis: Amyloidosis is a rare condition in which abnormal proteins (amyloids) build up in various organs, including the adrenal glands. This accumulation can disrupt adrenal function and cause Addison’s Disease.

Clinical Presentation of Addison’s Disease:
Due to Cortisol Deficiency:
- Addison’s Disease primarily results in the deficiency of cortisol, which is a crucial hormone for various bodily functions.
- Common symptoms due to cortisol deficiency include:
- Weakness: Individuals with Addison’s Disease often experience significant weakness, making even simple tasks challenging.
- Weight Loss: Unexplained weight loss can occur due to a disruption in metabolism.
- Fatigue: Profound fatigue and tiredness are typical, even after a full night’s sleep.
- Nausea and Vomiting: Persistent nausea and vomiting may be present.
- Diarrhea: Chronic diarrhea can develop as a result of gastrointestinal disturbances.
Due to Increased ACTH Production (If the Cause Is in the Adrenal Gland):
- When Addison’s Disease is caused by issues within the adrenal glands, it can lead to increased production of adrenocorticotropic hormone (ACTH).
- Symptoms related to excess ACTH include:
- Hyperpigmentation of Skin and Mucous Membranes: A distinctive symptom is the darkening of the skin and mucous membranes, which may appear as tan or bronze patches. This is often referred to as hyperpigmentation.
Due to Mineralocorticoid Deficiency:
- Addison’s Disease can also lead to the deficiency of mineralocorticoids, particularly aldosterone, which plays a crucial role in regulating electrolyte balance.
- Symptoms associated with mineralocorticoid deficiency include:
- Very Low Blood Pressure (Hypotension): The absence of aldosterone can result in extremely low blood pressure, leading to dizziness and fainting.
- Serum Potassium High, but Sodium and Chloride Are Low: Electrolyte imbalances can manifest as high levels of potassium and low levels of sodium and chloride.
Due to Androgen Deficiency:
- In some cases, Addison’s Disease may also cause androgen deficiency, which can lead to specific symptoms:
- Sparse Hair in Females: Women with Addison’s Disease may experience hair thinning or loss.
- General Weakness: Overexertion, exposure to cold, or acute infections can exacerbate the overall weakness and fatigue experienced by individuals with Addison’s Disease.
- In some cases, Addison’s Disease may also cause androgen deficiency, which can lead to specific symptoms:
Diagnosis of Addison’s Disease:
Hormone Levels Testing:
- To diagnose Addison’s Disease, healthcare providers typically start with hormone level testing. The key hormones involved are cortisol and ACTH (Adrenocorticotropic hormone).
- Morning and Evening Cortisol Levels: Blood samples are collected in the morning and evening to measure cortisol levels. In individuals with Addison’s Disease, both morning and evening cortisol levels are usually low.
- Plasma ACTH Level: Simultaneously, the level of ACTH in the blood plasma is measured. The results of this test help differentiate between primary and secondary adrenal insufficiency.
Differentiating Primary and Secondary Adrenal Insufficiency:
- In cases of primary adrenal insufficiency (due to issues with the adrenal glands themselves), ACTH levels are typically elevated (high), while cortisol levels are below normal.
- In secondary adrenal insufficiency (resulting from problems with the pituitary gland), both cortisol and ACTH levels are low.
ACTH Stimulation Test:
- In some cases, an ACTH stimulation test may be performed. In this test, a synthetic form of ACTH is administered, and blood cortisol levels are measured before and after the injection.
- A normal response to exogenous (administered from outside the body) ACTH involves a significant increase in blood cortisol levels.
- Individuals with Addison’s Disease often have a reduced or no increase in cortisol levels in response to ACTH stimulation.
Additional Blood Tests:
- Blood sugar levels and electrolyte values are also examined. Addison’s Disease can lead to imbalances in blood electrolytes, such as sodium and potassium, which can result in symptoms like weakness and low blood pressure.
Complications of Addison’s Disease:
Renal Failure:
- One of the potential complications of Addison’s Disease is renal failure, which refers to the loss of kidney function.
- Addison’s Disease can disrupt the balance of electrolytes in the body, particularly causing increased levels of potassium. This imbalance can have a detrimental effect on the kidneys.
- High levels of potassium can lead to abnormal heart rhythms (arrhythmias) and, in severe cases, impair kidney function.
Adrenal Hemorrhage:
- Adrenal hemorrhage, though rare, is another complication that can occur in individuals with Addison’s Disease.
- It involves bleeding into the adrenal glands, typically due to an adrenal crisis or severe stress. This can lead to sudden and severe abdominal or back pain.
- Adrenal hemorrhage requires immediate medical attention, as it can be life-threatening.
Addisonian Crisis:
- An Addisonian crisis, also known as an adrenal crisis, is a severe and potentially life-threatening complication of Addison’s Disease.
- It occurs when the adrenal glands fail to produce enough cortisol to meet the body’s needs, often triggered by stress, illness, trauma, or abrupt cessation of corticosteroid medications.
- Symptoms of an Addisonian crisis can include extreme weakness, confusion, low blood pressure, rapid heart rate, and even loss of consciousness.
- Prompt emergency medical treatment is essential to stabilize the patient, typically through intravenous administration of cortisol and fluids.
Depression:
- Chronic illnesses like Addison’s Disease can lead to emotional and psychological challenges, including depression.
- Coping with the demands of managing a chronic condition, along with the physical symptoms and potential complications, can take a toll on a person’s mental health.
- It’s essential for individuals with Addison’s Disease to receive comprehensive care that includes addressing emotional well-being and providing support for mental health issues such as depression.
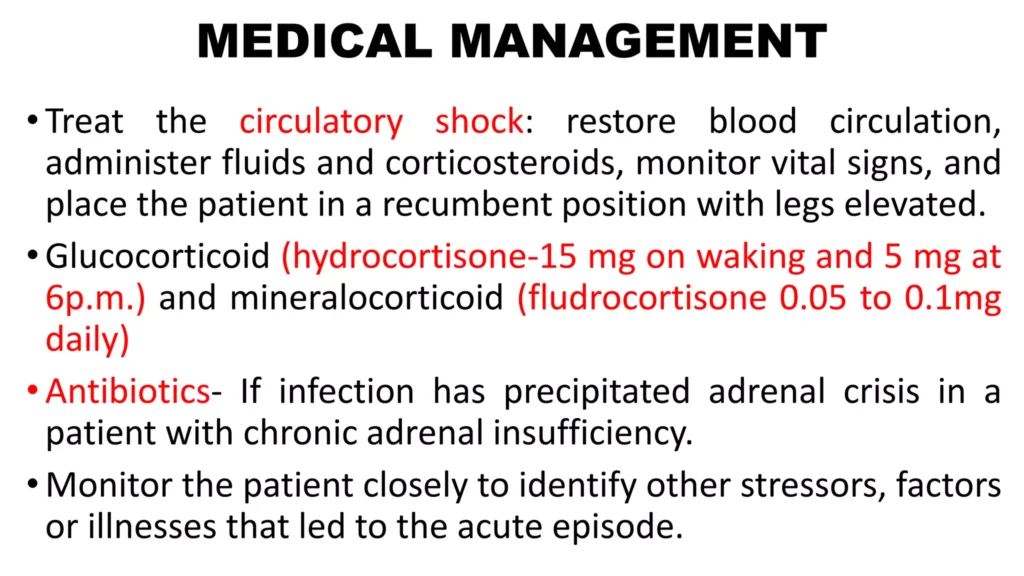

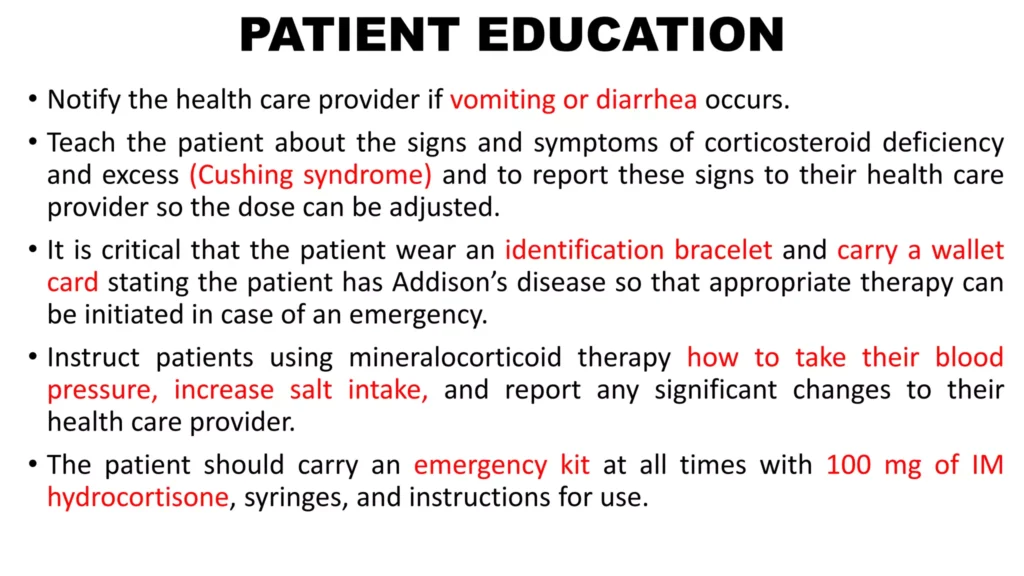
Medical Management
- Restore blood circulation IV fluids NS and Dextrose.
- Small dose of fludrocortisones 0.05 – 0.1mg/day is given to maintain BP and electrolytes
- Hormone replacement with cortisone daily in divided doses i.e prednisolone 20mg in the morning and 10mg in the evening
- Vasopressor amines may be required if hypertension persists.
- Antibiotic therapy if infection has precipitated the adrenal crisis
- Lifelong replacement of corticosteroids and mineralocorticoids.
- ORS for salt replacement.
- May need additional salt intake
- Treat underlying cause ie TB
Nursing Care
- Monitor for BP,P, as patient moves from lying, sitting, and standing position to asses for inadequate fluid volume.
- Assess skin color and turgor
- Assess history of weight changes, muscle weakness, and fatigue.
- Ask patient and family about onset of illness or increased stress that may have precipitated the crisis
Nursing diagnosis
- Electrolyte imbalance related to low sodium level as evidenced by craving for salt, vomiting and diarrhea.
- Ineffective tissue perfusion related to hyperpigmentation of skin as evidenced by skin tanning.
- Risk for fluid volume deficit related to vomiting and diarrhea.
.