Clostridium botulinum is a Gram-positive, strict-anaerobic, motile, pleomorphic, catalase-negative, endospore-forming bacillus (rod) that is ubiquitously found in the soil. The endopores of C. botulinum are sub-terminally placed or located on the bacterium and they are oval in shape. C. botulinum is found in the genus Clostridium and class Clostridia; and members are known to cause food spoilage, gas gangrene, botulism and tetanus. Clostridium species are able to ferment a wide variety of organic compounds, and they produce butyric acid, acetic acid, butanol and acetone, and large amounts of gas (CO2 and H2) as end products during the fermentation of sugars.
The ability of Clostridium species to produce gas under anaerobic conditions is the reason why most canned foods contaminated by the pathogen are swollen. It is the causative agent of botulism, a non-communicable disease and a type of food poisoning caused by the exotoxin produced by C. botulinum. Some Clostridium species are also found in water and mammalian/animal intestinal tract and, they are known to also grow in food if the environmental condition of the food is suitably anaerobic or anoxic. Notably, the pathogen is notorious for growing in vacuum-packed or canned food that inherently has anoxic environment due to inappropriate sterilization.
The exotoxins produced by C. botulinum are specifically neurotoxins (types A – G) that affect the central nervous system (CNS) of its host by inhibiting stimulus transmission to the motor end plates of the neurons/nerves, thus preventing key muscular contractions in the body. The endopores and/or exotoxins produced by C. botulinum are heat labile/resistant, and thus sufficient amount of heating is required to destroy or inactivate the pathogen. Other important members of the genus Clostridium that are of clinical importance aside C. botulinum include C. tetani (causative agent of tetanus) and C. perfringens (causative agent of gas gangrene). C. tetani produces tetanospasmin (tetanus toxin) that causes tetanus and lock-jaw (in rare and serious infections) in humans.
In effect, Clostridium species (especially C. tetani and C. botulinum) produce the most potent biological toxins known to affect humans. It is however noteworthy that most species of Clostridium are apathogenic saprophytes (i.e. non-infectious microbes) that live in the soil where they degrade organic matters. Most notably is the fact that Clostridium species produce a wide variety of extracellular enzymes that allows them to efficiently degrade macromolecules such as proteins, lipids, collagen, and cellulose. This property makes them putative agents of biodegradation in the environment.
PATHOGENESIS OF CLOSTRIDIUM BOTULINUM INFECTION
Food-borne botulism or C. botulinum infection in humans occurs following the ingestion of food containing preformed exotoxins (neurotoxin) formed by the pathogen. When home-made canned foods are not properly or well heated to kill the contaminating endopores of C. botulinum, food-intoxication is bound to occur in the individual. Most foods that are eaten almost raw i.e. without cooking are mainly the once with contaminating endospores of C. botulinum. Once these foods become contaminated by the pathogen, C. botulinum grows anaerobically to produce its exotoxin. C. botulinum produces seven types of exotoxins (A – G), but human infections are basically caused by the toxigenic types: A, B, E and F. The environment (soil) is the main source of infection with C. botulinum.
Despite the danger posed by the ingestion of C. botulinum exotoxin, properly cooked or heated foods (100oC for 10 mins) are safe to eat if they previously contained the pre-formed toxin since high temperature deactivates it. After ingestion of the exotoxins, the toxin is absorbed by the gastrointestinal tract (GIT) from where it is transported to the peripheral nervous system. Notably, C. botulinum neurotoxin blocks neuroexocytosis of vesicles containing acetylcholine (a neurotransmitter). This phenomenon goes on to prevent nervous stimulation of the host’s muscles that leads to a flaccid paralysis that resembles that caused by tetanus infection but without muscle contractions.
Spasm is used for tetanus infection while paralysis is used to describe botulism. Normally, a flaccid (weak) type of paralysis ensues within day 1 to 2 in the host. Other clinical signs and symptoms of botulism may include dizziness, weakness, blurred vision, dryness of the mouth, descending weakness of skeletal muscles, vomiting, diarrhea, aphonia (loss of voice) and respiratory arrest in infant botulism. The incubation period of the disease depends on whether the exotoxin was ingested pre-formed, via wound or endogenously in the GIT of infants or neonates and on the quantity of toxins that entered the body. Botulism in humans can present clinically in various forms including infant botulism, wound botulism and adult (food-borne) botulism.
Infant botulism is a type of intoxication caused by the ingestion of C. botulinum endospores from the environment. In infant botulism, the endospores grow in the normal flora of the infant’s GIT which is not yet fully formed or developed as is the case in adults. The exotoxin is produced in vivo after the entry of the endospores. Non-sterile honeys may also introduce the toxins of C. botulinum into the GIT of infants. Adult botulism is caused by the ingestion of pre-formed exotoxins in food contaminated by C. botulinum. Examples of food that may be contaminated by the pathogen include smoked fishes, poorly canned foods and vegetables.
Endospores of C. botulinum normally found in the soil are not properly killed during canning, and this allows the pathogen to germinate during storage to produce exotoxins which are ingested by human hosts. Wound botulism though rare is caused by the traumatic implantation of C. botulinum endospores into the host’s body. This usually occurs during accidents, abrasion or pricking of the body with sharp objects that has been soil-contaminated.
LABORATORY DIAGNOSIS OF CLOSTRIDIUM BOTULINUM INFECTION
The laboratory diagnosis of C. botulinum food-intoxication (botulism) is by the identification of the pathogen in contaminated food samples, intestinal contents and detection of the organism’s toxin in blood (serum) samples of infected individuals. Stool, vomitus and tissue samples can also be obtained from the patients depending on the type of botulism being investigated. Serum is irrelevant in detecting infant botulism in neonates.
Notably, in vivo studies using laboratory animals (e.g. mice) can be conducted in very strong cases of botulism to establish the presence of the bacterial toxin. Mice injected intraperitoneally with the serum of infected patients die instantaneously, and this is a strong indication that the food contained preformed exotoxins of C. botulinum. Haemagglutination assays are basically used to demonstrate the toxins of C. botulinum in the serum of infected patients.
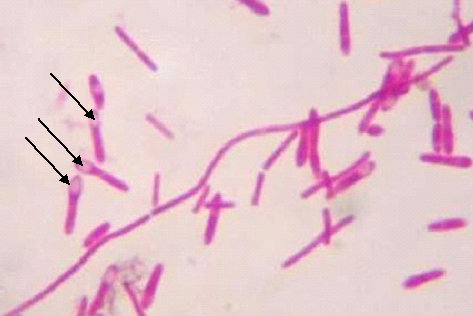
The causative agent of botulism is not usually cultured but suspect food samples containing C. botulinum can be cultured in specialized selective media such as the Robertson’s cooked meat medium (RCMM) and the lactose egg yolk milk agar under anaerobic conditions at 35oC for about 2-5 days. Identification of the spores of C. botulinum in a stained preparation can also be employed in the presumptive detection of the pathogen (Figure 1).
IMMUNITY TO CLOSTRIDIUM BOTULINUM INFECTION
Protective or long-lasting immunity to botulism does not develop even with severe cases of the disease. The intravenous injection of the antitoxin has the potential to neutralized toxins that have not yet bind to the nerve endings of the host. Thus, persons known to have ingested food with C. botulinum contamination should be treated immediately with antiserum. Scientists working in Reference Laboratories and on C. botulinum have experimental vaccines that protect them from the pathogen.
TREATMENT OF CLOSTRIDIUM BOTULINUM INFECTION
Supportive care is mainly needed to manage food intoxication caused by C. botulinum. However, a polyvalent antitoxin (of equine origin) is administered intravenously with carefulness. But this antitoxin/antiserum is rarely used in some clinical conditions due to the allergic reactions it sparks in patients (especially infants). Respiratory failures (or pharyngeal paralysis) can cause mortality thus proper ventilation should be maintained in all cases using an artificial breathing apparatus to supply oxygen. On the contrary, most cases of infant botulism are self limiting, and neonates recover from the infection when given proper supportive care. Antibiotics (e.g. amoxicillin) can be administered in cases of wound botulism.
PREVENTION AND CONTROL OF CLOSTRIDIUM BOTULINUM INFECTION
Though food intoxication caused by C. botulinum is an uncommon disease, the prevention of botulism is important and lies in the proper cooking of our foods. Since adequate pressure cooking and autoclaving kills the endopores of C. botulinum, these measures must always be applied to in the processing of our foods. Only heating foods for 10 mins at 100oC kills the endospores of the pathogen.
Foods in swollen or damaged cans should not be eaten but rather destroyed immediately because C. botulinum toxins could be deadly once ingested. Infants should not be given honey in their first years since it could serve as a route via which the toxin reaches their GIT whose normal flora is still developing. Proper food hygiene during the handling and preparation/processing of food is the most important way of preventing food intoxication (botulism) in human population.
OTHER SPECIES OF CLOSTRIDIUM
- C. tetani: C. tetani is the causative agent of tetanus infection in humans.
- C. cadaveris: C. cadaveris is usually considered non-pathogenic and it does not produce toxins like other species of Clostridium. C. cadaveris is found in soil, water, and as a normal component of the human intestinal tract; and infections due to C. cadaveris in humans are rare. The organism is seldom found is clinical specimens; and may cause infections in immunocompromised hosts.
- C. acidurici: C. acidurici is an anaerobic, homoacetogenic bacterium, which is able to use purines such as uric acid as sole carbon, nitrogen, and energy source. It is found in the environment; and the organism is resistant to some antibiotics including bacitracin.
- C. cellobioparum: C. cellobioparum is an anaerobic cellulose-degrading Gram-positive bacterium found in the bovine rumen.
- C. kluyveri: C. kluyveri is a strict anaerobe with unique metabolic features; and it grows anaerobically on ethanol and acetate as sole energy sources to produce metabolic products such as hydrogen, butyrate, and caproate. The organism has been used in the past as a source of enzymes; and it produces a variety of enzymes including phosphotransacetylase (used for analytical purposes) and enoate reductases (used for stereo-specific hydrogenation reactions).
- C. butyricum: C. butyricum is a strict-anaerobic endospore forming species of Clostridium that produces butyric acid via fermentation. Medically, it interferes with the growth of Clostridium difficile by antagonizing its multiplication; and thus is used in some hospitals to treat C. difficile infections. C. butyricum effectively convert glycerol to 1,3-propanediol.
- C. perfringens: C. perfringens is the causative agent of gas gangrene in humans; and it is implicated in some tissue necrosis and bacteraemia. It is a common cause of foodborne illness in human population. C. perfringens is ubiquitous in nature and can be found as a normal component of decaying vegetation, the intestinal tract of humans and other vertebrates, insects, and soil.
- C. propionicum: C. propionicum is commonly isolated from the environment; and it is of immense industrial importance because of its metabolic products including acetate, ammonia, carbon dioxide and propionate – which it produces via fermentation.
- C. aceticum: C. aceticum is an acetogenic bacterium and endospore-forming species of Clostridium that produces acetic acid. It is able to grow autotrophically on a CO2 plus H2 gas mixture as well as heterotrophically on sugars, organic acids, and alcohols.
- C. acetobutylicum: C. acetobutylicum is a soil-dwelling species of Clostridium that naturally produces acetone as well as butanol and ethanol. Industrially, it is used for solvent production. The organism is saccharolytic in nature (i.e. it can break down sugar).
- C. histolyticum: C. histolyticum is a species of Clostridium that is abundantly found in feaces and in the soil; and it is pathogenic in guinea pigs, mice, rabbits, and humans. It produces five toxins including alpha, beta, gamma, delta, and epsilon toxins responsible for its toxigenicity; and these exotoxins have proteolytic and necrotizing properties that cause severe local necrosis in humans. C. histolyticum produces collagenase which destroys connective tissue of muscles.
- C. sporogenes: C. sporogenes is found soil and sediments in both marine and freshwater environments, and in other products such as preserved meat and dairy products, feacal matter. It lacks the capability to produce the neurotoxin, botulinum that causes human disease; and the organism does not carry plasmids that are responsible for neurotoxicity of Clostridium species. C. sporogenes is usually a harmless species of Clostridium.
- C. difficile: C. difficileisa spore-forming bacteriumthat causes diarrhea. It produces enterotoxins and cytotoxins that produce diarrhea and inflammation in infected human hosts. It can colonize the human gut and human infection is usually via the feacal-oral-route.
References
Brooks G.F., Butel J.S and Morse S.A (2004). Medical Microbiology, 23rd edition. McGraw Hill Publishers. USA. Pp. 248-260.
Madigan M.T., Martinko J.M., Dunlap P.V and Clark D.P (2009). Brock Biology of microorganisms. 12th edition. Pearson Benjamin Cummings Publishers. USA. Pp.795-796.
Prescott L.M., Harley J.P and Klein D.A (2005). Microbiology. 6th ed. McGraw Hill Publishers, USA. Pp. 296-299.
Ryan K, Ray C.G, Ahmed N, Drew W.L and Plorde J (2010). Sherris Medical Microbiology. Fifth edition. McGraw-Hill Publishers, USA.
Singleton P and Sainsbury D (1995). Dictionary of microbiology and molecular biology, 3rd ed. New York: John Wiley and Sons.
Talaro, Kathleen P (2005). Foundations in Microbiology. 5th edition. McGraw-Hill Companies Inc., New York, USA.
