abruptio placentae
Also found in: Dictionary, Thesaurus, Wikipedia.
abruptio
[ab-rup´she-o] (L.)Contributing factors include multiple pregnancies (grand multiparity), chronic hypertensive disease, direct trauma to the uterus, or sudden release of amniotic fluid.
Premature separation of the placenta is classified from Grade 0 to Grade 3 according to the degree of separation. In Grade 0 mother and fetus are asymptomatic. Diagnosis is made after delivery when the placenta is examined and a clot is found adhering to the maternal surface. Grade 1 is minimal separation that causes some vaginal bleeding and changes in maternal vital signs. Fetal distress and hemorrhagic shock are absent. Grade 2 is moderate separation in which there is evidence of fetal distress and maternal symptoms of a tense uterus and pain on palpation. Grade 3 is the most serious. There is extreme separation which, without prompt intervention, can lead to maternal shock and fetal death.

Oxygen may be administered to the mother to limit fetal anoxia. Fetal heart sounds are monitored for signs of fetal distress. The patient is kept in a lateral rather than supine position during labor to prevent pressure on the vena cava and further inhibition of fetal blood supply. Vaginal or pelvic examinations and an enema are restricted lest the placenta be disturbed further.
Grade 2 and Grade 3 separations require delivery as soon as possible, either vaginally or by cesarean section. Without prompt and effective intervention, abruptio placentae can lead to maternal death from hemorrhage, shock, and circulatory collapse. Fetal prognosis depends on the extent of hypoxia suffered by the fetus during labor and delivery.
ab·rup·ti·o pla·cen·tae
(ab-rŭp'shē-ō pla-sen'tē), Avoid the misspelling/mispronunciation abruptio placenta.abruptio placentae
The premature separation of the placenta from its site of implantation in the endometrium before the delivery of the foetus, commonly known as placental abruption. Some degree of AP occurs in 1:85 deliveries; severe AP with total separation of the placenta is an obstetric emergency seen in 1 in 500–750 deliveries, often accompanied by foetal death.Clinical findings
Abdominal and/or back pain; irritable, tender or hypertonic uterus; vaginal bleeding (seen in most); 30% are asymptomatic.
Predisposing factors
Pre-eclampsia, eclampsia, chronic hypertension, diabetes, chronic renal disease; mechanical causes are rare (1–5%) and include transabdominal trauma, sudden decompression (as occurs in the delivery of a 1st twin or rupture of membranes in hydramnios) or traction of a short placenta.
Pathophysiology, proposed mechanisms
Local vascular injury of the decidua basalis with bleeding and haematoma formation, which causes shearing of adjacent denuded vessels, exacerbating the bleeding and haematoma; abrupt increased in uterine venous pressure transmitted to intervillous space, resulting in venous bed engorgement and separation of part or the entire placenta.
Management
Expectant therapy if foetus is immature and bleeding limited, treat shock if present; vaginal delivery if possible, or else C-section.
Complications
DIC, acute cor pulmonale, renal cortical and tubular necrosis, uterine apoplexy, transfusion hepatitis.
Definable, direct causes that trigger placenta abruptio
Rare (1 to 5%) mechanical factors such as abdominal trauma (for example, from an automobile accident or fall), sudden loss in uterine volume as occurs with rapid loss of amniotic fluid or the delivery of a first twin, or an abnormally short umbilical cord (usually only a problem at the time of delivery). Predisposing factors include the following risk factors: a past medical history of placenta abruptio (after 1 prior episode there is a 10 to 17% recurrence; after 2 prior episodes the incidence of recurrence exceeds 20%); hypertension during pregnancy is associated with up to 18% incidence (however, approximately 50% of placenta abruptio cases severe enough to cause foetal death are associated with hypertension); increased maternal age; increased number of prior deliveries; increased uterine distention (as may occur with multiple pregnancies or abnormally large volume of amniotic fluid); diabetes mellitus in the pregnant woman; cigarette smoking; and drinking alcohol during pregnancy (> 14 drinks per week). The incidence of placenta abruptio, including any amount of placental separation prior to delivery, is about 1 out of 77–89 deliveries; however, the severe form (resulting in foetal death) occurs only in about 1 out of 500–750 deliveries.
abruptio placentae
Ablatio placentae, abruptio, premature separation of placenta Obstetrics The premature separation of the placenta from its site of implantation in the endometrial before the delivery of the fetus; some degree of AP occurs in 1:85 deliveries; severe AP with total separation of the placenta is an obstetric emergency which occurs about 1 in 500-750 deliveries, and is accompanied by fetal death Clinical Constant abdominal and/or back pain, irritable, tender or hypertonic uterus, vaginal bleeding—seen in most; 30% are asymptomatic Predisposing factors Preeclampsia-eclampsia, chronic HTN, DM, chronic renal disease; mechanical causes are rare–1-5% and include transabdominal trauma, sudden decompression, as occurs in the delivery of a 1st twin or rupture of membranes in hydramnios, or traction of a short placenta Management Expectant therapy if fetus is immature and bleeding limited, treat shock if present, vaginal delivery if possible, C-section Complications DIC, acute cor pulmonale, renal cortical and tubular necrosis, uterine apoplexy, transfusion hepatitis.ab·rup·ti·o pla·cen·tae
(ăb-rŭp'shē-ō plă-sen'tē)abruptio placentae
Etiology
The cause is unknown; however, the condition is most commonly associated with pregnancy-induced hypertension (PIH). It may occasionally be related to abdominal trauma, substance abuse (cigarette, alcohol, or cocaine), or sudden premature rupture of membranes.
Symptoms
Abruptio placentae is classified according to type and severity. Grade 1: vaginal bleeding with possible uterine tenderness and mild tetany; neither mother nor baby is in distress; approximately 10% to 20% of placental surface is detached. Grade 2: uterine tenderness; tetany, with or without uterine bleeding; fetal distress; mother is not in shock. Approximately 20% to 50% of the total surface area of the placenta is detached. Grade 3: Uterine tetany is severe; the mother is in shock, although bleeding may be covert; and the fetus is dead. Often the patient develops coagulopathy. More than 50% of the placental surface is detached.
Pathology
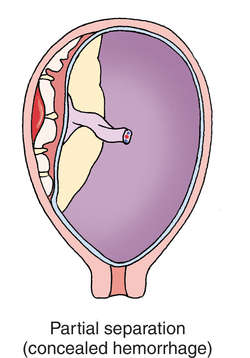
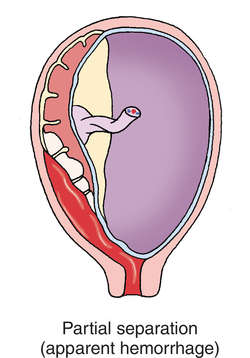
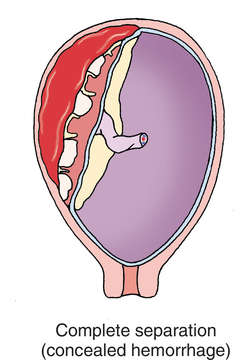
Extravasation of blood occurs between the placenta and the uterine wall, occasionally between muscle fibers of the uterus. Hemorrhage can be concealed or covert, causing consumptive coagulopathy (disseminated intravascular coagulopathy).
Treatment
This varies with the type and extent of abruption. Women experiencing only a small marginal separation of the placenta from the uterine wall may be confined to bed and monitored closely for signs of further threat to maternal or fetal status. If prematurity also is a factor, the woman may be given betamethasone to expedite development of fetal pulmonary surfactant. If the woman is at or near term, induction of labor and vaginal delivery may be an option. See: betamethasone
Supportive treatment and prompt surgical intervention are indicated for women who have moderate to severe abruptions. Complete detachment calls for immediate cesarean delivery, concomitant treatment of shock and, sometimes, management of a coagulation defect. The massive loss of blood jeopardizes the mother's survival; fetal mortality is 100%. If the uterus fails to contract after the surgical delivery, immediate hysterectomy may be necessary. See: Couvelaire uterus
Prognosis
Although maternal mortality is unusual, other than as noted, the perinatal mortality is between 20% and 30%.
Patient care
Early recognition and prompt management of the event and any associated complications are vital. The woman's vital signs, fundal height, uterine contractions, labor progress, and fetal status data are monitored, including heart rate and rhythm. Any changes are noted, such as prolonged decelerations in fetal heart rate or alterations in baseline variability; uterine tetany; complaints of sudden, severe abdominal pain; and the advent of or increase in vaginal bleeding. Vaginal blood loss is estimated by weighing perineal pads and subtracting the known weight of dry pads. The interval between pad changes, the character and amount of the bleeding, and the degree of pad saturation are noted. Prescribed IV fluids and medications are administered through a large-bore catheter. A central venous pressure line may be placed to provide access to the venous circulation, and an indwelling catheter is inserted to monitor urinary output and fluid balance. A calm atmosphere is maintained, and the patient's verbalization is encouraged. The patient is assisted in coping with her fears and anxiety. Questions are answered truthfully, comfort measures are implemented, and reassurance is provided as possible and consistent with the current situation and prognosis. All procedures are explained, and the woman and her family are prepared for induction of labor, vaginal delivery, or cesarean birth, as appropriate. The woman must be assured that everything is being done for the neonate's survival, which depends primarily on gestational age, blood loss, and associated hypertensive disorders.
abruptio placentae
Premature detachment of the PLACENTA from the wall of the womb (UTERUS).Abruptio Placentae
| DRG Category: | 774 |
| Mean LOS: | 3.3 days |
| Description: | MEDICAL: Vaginal Delivery with Complicating Diagnoses |
Abruptio placentae is the premature separation of a normally implanted placenta before the delivery of the baby. It is characterized by a triad of symptoms: vaginal bleeding, uterine hypertonus, and fetal distress. It can occur during the prenatal or intrapartum period. In a marginal abruption, separation begins at the periphery and bleeding accumulates between the membranes and the uterus and eventually passes through the cervix, becoming an external hemorrhage. In a central abruption, the separation occurs in the middle, and bleeding is trapped between the detached placenta and the uterus, concealing the hemorrhage. Frank vaginal bleeding also does not occur if the fetal head is tightly engaged. Since bleeding can be concealed, note that the apparent bleeding does not always indicate actual blood loss. If the placenta completely detaches, massive vaginal bleeding is seen. Abruptions are graded according to the percentage of the placental surface that detaches (see Table 1). Visual inspection of an abrupted placenta reveals circumscribed depressions on its maternal surface and is covered by dark, clotted blood. Destruction and loss of function of the placenta result in fetal distress, neurological deficits such as cerebral palsy, or fetal death.
| Grade 0 | Less than 10% of the total placental surface has detached; the patient has no symptoms; however, a small retroplacental clot is noted at birth. |
| Grade I | Approximately 10%–20% of the total placental surface has detached; vaginal bleeding and mild uterine tenderness are noted; however, the mother and fetus are in no distress. |
| Grade II | Approximately 20%–50% of the total placental surface has detached; the patient has uterine tenderness and tetany; bleeding can be concealed or is obvious; signs of fetal distress are noted; the mother is not in hypovolemic shock. |
| Grade III | More than 50% of the placental surface has detached; uterine tetany is severe; bleeding can be concealed or is obvious; the mother is in shock and often experiencing coagulopathy; fetal death occurs. |
Causes
The cause of abruptio placentae is unknown; however, any condition that causes vascular changes at the placental level may contribute to premature separation of the placenta. Hypertension, preterm premature rupture of membranes, smoking, maternal trauma, trauma related to intimate partner violence, and cocaine abuse are the most common associated factors. A short umbilical cord, thrombophilias, fibroids (especially those located behind the placental implantation site), severe diabetes or renal disease, advanced maternal age, and vena caval compression are other predisposing factors. Chronic upper respiratory infections and chronic bronchitis also increase the incidence of abruptio placentae.
Genetic considerations
No clear genetic contributions to susceptibility have been defined.
Gender, ethnic/racial, and life span considerations
Increased incidence of abruption is noted in those with multiparity, in pregnant women over 40, and for those with a history of past abruptio placentae. Abruptions occur in 1 of 200 deliveries and are responsible for 10% of third-trimester stillbirths. Severe abruptions are associated with a 25% to 35% perinatal mortality rate. While abruptio placentae is more common in African American women than in white or Latina women, experts are unsure of the cause of these differences.
Global health considerations
Experts estimate that abruptio placentae occurs in 1% of all pregnancies regardless of country or origin.
Assessment
History
Obtain an obstetric history. Determine the date of the last menstrual period to calculate the estimated day of delivery and gestational age of the infant. Inquire about alcohol, tobacco, and drug usage and any trauma or abuse situations during pregnancy. Ask the patient to describe the onset of bleeding (the circumstances, amount, and presence of pain). When obtaining a history from a patient with an abruption, recognize that it is possible for her to be disoriented from blood loss and/or cocaine or other drug usage. Generally, patients have one of the risk factors, but sometimes no clear precursor is identifiable.
Physical examination
The most common symptoms include vaginal bleeding, abdominal or back pain and tenderness, fetal distress, and abnormal uterine contractions. Assess the amount and character of vaginal bleeding; blood is often dark red in color, and the amount may vary depending on the location of abruption. Palpate the uterus; patients complain of uterine tenderness and abdominal/back pain. The fundus is woodlike, and a poor resting tone can be noted. With a mild placental separation, contractions are usually of normal frequency, intensity, and duration. If the abruption is more severe, strong, erratic contractions occur. Assess for signs of concealed hemorrhage: slight or absent vaginal bleeding; an increase in fundal height; a rigid, boardlike abdomen; poor resting tone; constant abdominal pain; and late decelerations or decreased variability of the fetal heart rate. A vaginal examination should not be done until an ultrasound is performed to rule out placenta previa.
Using electronic fetal monitoring, determine the baseline fetal heart rate and presence or absence of accelerations, decelerations, and variability. At times, persistent uterine hypertonus is noted with an elevated baseline resting tone of 20 to 25 mm Hg. Ask the patient if she feels the fetal movement. Fetal position and presentation can be assessed by Leopold’s maneuvers. Assess the contraction status and view the fetal monitor strip to note the frequency and duration of contractions. Throughout labor, monitor the patient’s bleeding, vital signs, color, urine output, level of consciousness, uterine resting tone and contractions, and cervical dilation. If placenta previa has been ruled out, perform sterile vaginal examinations to determine the progress of labor. Assess the patient’s abdominal girth hourly by placing a tape measure at the level of the umbilicus. Maintain continuous fetal monitoring.
Psychosocial
Assess the patient’s understanding of the situation and also the significant other’s degree of anxiety, coping ability, and willingness to support the patient. Assess the patient for intimate partner violence or other violence in the home.
Diagnostic highlights
General Comments: Abruptio placentae is diagnosed based on the clinical symptoms, and the diagnosis is confirmed after delivery by examining the placenta.
| Test | Normal Result | Abnormality With Condition | Explanation |
|---|---|---|---|
| Pelvic ultrasound | Placenta is visualized in the fundus of the uterus | None; ultrasound is used to rule out a previa | If the placenta is in the lower uterine segment, a previa (not an abruption) exists; while ultrasonography helps to determine the location of the placenta, it is not always useful in diagnosing abruptio placentae. A normal sonogram does not exclude the condition. |
Other Tests: Complete blood count; coagulation studies; type and crossmatch; magnetic resonance imaging; a nonstress test and biophysical profile are done to assess fetal well-being.
Primary nursing diagnosis
Diagnosis
Fluid volume deficit related to blood lossOutcomes
Fluid balance; Hydration; Circulation statusInterventions
Bleeding reduction; Blood product administration; Intravenous therapy; Shock managementPlanning and implementation
Collaborative
If the fetus is immature (< 37 weeks) and the abruption is mild, conservative treatment may be indicated. However, conservative treatment is rare because the benefits of aggressive treatment far outweigh the risk of the rapid deterioration that can result from an abruption. Conservative treatment includes bedrest, tocolytic (inhibition of uterine contractions) therapy, oxygen, and constant maternal and fetal surveillance. Generally an intravenous (IV) line should be started and a type and crossmatch completed in case of the need for administration of IV fluids and/or blood. Rho(D) immune globulin (RhoGAM) is given if the patient is Rh-negative due to the increased chance of fetal cells entering the maternal circulation. If a vaginal delivery is indicated and no regular contractions are occurring, the physician may choose to infuse oxytocin cautiously in order to induce the labor.
If the patient’s condition is more severe, aggressive, expedient, and frequent assessments of blood loss, vital signs, and fetal heart rate pattern and variability are performed. Give a lactated Ringer’s solution IV via a large-gauge peripheral catheter. At times, two IV catheters are needed, especially if a blood transfusion is anticipated and the fluid loss has been great. If there has been an excessive blood loss, blood transfusions and central venous pressure (CVP) monitoring may be ordered. A normal CVP of 10 cm H2O is the goal. CVP readings may indicate fluid volume deficit (low readings) or fluid overload and possible pulmonary edema following treatment (high readings).
If the mother or fetus is in distress, an emergency cesarean section is indicated. If any signs of fetal distress are noted (flat variability, late decelerations, bradycardia, tachycardia), turn the patient to her left side, increase the rate of her IV infusion, administer oxygen via face mask, and notify the physician. If a cesarean section is planned, see that informed consent is obtained in accordance with unit policy, prepare the patient’s abdomen for surgery, insert a Foley catheter, administer preoperative medications as ordered, and notify the necessary personnel to attend the operation.
After delivery, monitor the degree of bleeding and perform fundal checks frequently. The fundus should be firm, midline, and at or below the level of the umbilicus. Determine the Rh status of the mother; if the patient is Rh-negative and the fetus is Rh-positive with a negative Coombs’ test, administer RhoGAM.
Pharmacologic highlights
| Medication or Drug Class | Dosage | Description | Rationale |
|---|---|---|---|
| Magnesium sulfate | 4–6 g IV loading dose, 1–4 g/hr IV maintenance | Anticonvulsant | Effective tocolytic; relaxes the uterus, slowing the abruption |
| Oxytocin (Pitocin) | 10–20 U in 500–1,000 mL of IV fluid | Oxytocic | Assists the uterus to contract after delivery to prevent hemorrhage |
Independent
During prenatal visits, explain the risk factors and the relationship of alcohol and substance abuse to the condition. Teach the patient to report any signs of abruption, such as cramping and bleeding. If the patient develops abruptio placentae and a vaginal delivery is chosen as the treatment option, the mother may not receive analgesics because of the fetus’s prematurity; regional anesthesia may be considered. The labor, therefore, may be more painful than most mothers experience; provide support during labor. Keep the patient and the significant others informed of the progress of labor as well as the condition of the mother and fetus. Monitor the fetal heart rate for repetitive late decelerations, decreased variability, and bradycardia. If noted, turn the patient on her left side, apply oxygen, increase the rate of the IV, and notify the physician immediately.
Offer as many choices as possible to increase the patient’s sense of control. Reassure the significant others that both the fetus and the mother are being monitored for complications and that surgical intervention may be indicated. Provide the patient and family with an honest commentary about the risks. Discuss the possibility of an emergency cesarean section or the delivery of a premature infant. Answer the patient’s questions honestly about the risk of a neonatal death. If the fetus does not survive, support the patient and listen to her feelings about the loss.
Evidence-Based Practice and Health Policy
Arnold, D.L., Williams, M.A., Miller, R.S., Qiu, C., & Sorensen, T.K. (2009). Iron deficiency anemia, cigarette smoking and risk of abruptio placentae. Journal of Obstetrics and Gynaecology Research, 35(3), 446–452.
- A retrospective case-control study that compared 145 women with abruptio placentae to 1,710 randomly selected control subjects revealed significant associations between abruption placentae and maternal smoking, hypertension, and iron deficiency anemia.
- A greater proportion of women with abruptio placentae smoked during their pregnancy (15.4% versus 6.9%) and had pregestational hypertension (11% versus 2.6%) when compared to the control sample (p < 0.05). In this study, smoking during pregnancy increased the odds of abruptio placentae by 2.48 times (95% CI, 1.58 to 4.25).
- Maternal iron deficiency anemia also increased the odds of abruptio placentae by 3.6 times (95% CI, 2.01 to 6.04). Being both a smoker and having anemia increased the odds by 4.29 (95% CI, 0.90 to 20.51).
Documentation guidelines
- Amount and character of bleeding: Uterine resting tone; intensity, frequency, and duration of contractions and uterine irritability
- Response to treatment: Intravenous fluids, blood transfusion, medications, surgical interventions
- Fetal heart rate baseline, variability, absence or presence of accelerations or decelerations, bradycardia, tachycardia
Discharge and home healthcare guidelines
Discharge before delivery (if the fetus is very immature and the mother and infant are stable).