History and Physical Examination
Infants with gastroschisis and omphalocele can be identified by prenatal ultrasonography. [30] Defects in other organ systems may also be diagnosed, and chromosomal abnormalities may be discovered by amniocentesis. See Workup.
Omphalocele
In an omphalocele, the diameter of the abdominal wall defect varies between 4 and 12 cm; the defect is located centrally, or in the epigastrium or the hypogastrium.
With a large omphalocele, dystocia may occur and cause liver injury.
The omphalocele sac is ruptured in 10%-20% of cases; rupture may occur in utero or during delivery.
Infants with Beckwith-Wiedemann syndrome have the following characteristics:
-
Omphalocele (generally small)
-
Macroglossia and coarse, rounded facial features
-
Visceromegaly with hyperplasia of the pancreatic islet cells causing neonatal hypoglycemia, which may be severe
-
Genitourinary abnormalities
Increased incidence of Wilms tumors, liver tumors (hepatoblastoma), and adrenocortical neoplasms; surveillance by ultrasonography is indicated
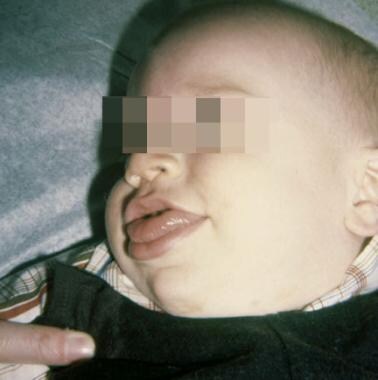 Pediatric omphalocele and gastroschisis (abdominal wall defects). Note the enlarged tongue in this infant with Beckwith-Wiedemann syndrome.
Pediatric omphalocele and gastroschisis (abdominal wall defects). Note the enlarged tongue in this infant with Beckwith-Wiedemann syndrome.
Pentalogy of Cantrell includes the following components [31] :
-
Epigastric omphalocele
-
Cleft sternum
-
Anterior (retrosternal) diaphragmatic hernia of Morgagni
-
Absent pericardium
-
Cardiac defects (ectopia cordis and ventricular septal defects)
Giant omphalocele features are as follows:
-
Large, centrally located, abdominal wall defect
-
Ectopic liver, located outside of the abdominal cavity, within the omphalocele sac
-
Small, undeveloped abdominal and thoracic cavities
-
Restrictive lung disease and pulmonary hypoplasia associated with the hypoplastic thoracic cavity
-
Best to accomplish operative closure in stages (to avoid excessive intra-abdominal pressure) [32]
Gastroschisis
The abdominal wall defect of gastroschisis is generally uniform in size (≤5 cm) and constant in location (right of the umbilical cord).
The amount of inflammation of the extruded intestine varies. Inflammation may be minimal, or it may distort the appearance of the bowel, obscuring the anatomy and making it difficult even to identify an atresia. See the images below.
 Pediatric omphalocele and gastroschisis (abdominal wall defects). Inflammatory distortion of the extruded intestine is shown. There appears to be an associated atresia (the dilated intestine), but the dilatation resolved in concert with resolution of the inflammation.
Pediatric omphalocele and gastroschisis (abdominal wall defects). Inflammatory distortion of the extruded intestine is shown. There appears to be an associated atresia (the dilated intestine), but the dilatation resolved in concert with resolution of the inflammation.
 Pediatric omphalocele and gastroschisis (abdominal wall defects). This infant has gastroschisis and colon atresia, with the proximal end open. An ostomy is brought out of the silo.
Pediatric omphalocele and gastroschisis (abdominal wall defects). This infant has gastroschisis and colon atresia, with the proximal end open. An ostomy is brought out of the silo.
 Pediatric omphalocele and gastroschisis (abdominal wall defects). The sac is removed, and the abdominal wall defect is closed around the in utero colostomy.
Pediatric omphalocele and gastroschisis (abdominal wall defects). The sac is removed, and the abdominal wall defect is closed around the in utero colostomy.
The amount of inflammation, the distribution of meconium (whether it can be evacuated manually through the anus), or whether succus entericus can be milked into the stomach and suctioned (by anesthesia), are factors that determine whether reduction and closure of the abdominal wall defect can be accomplished primarily or whether a "silo" must be used.
When primary closure of the abdominal wall defect is not possible, a silo is utilized to contain the intestine until the inflammation has resolved and it becomes soft and pliable. Usually, reduction be accomplished within 1 week. Correction of intestinal atresia, by either an anastomosis or an enterostomy, is best delayed until closure of the abdominal cavity has been achieved.
Intestinal dysfunction, delaying the onset of feedings, may take 4-6 weeks to resolve.
When gastroschisis is identified antenatally, serial ultrasonography is performed to identify compromise to the intestinal viability.
Concomitantly, amniocentesis monitors lung maturity and signals when to induce labor. [33, 34, 35, 36, 37]
Cloacal exstrophy
Characteristics of cloacal exstrophy include the following:
-
Bladder exstrophy with a central strip (plate of cecum) and prolapsed ileum (elephant trunk appearance)
-
Potential presence of duplication of the colon and appendix, or colonic atresia, or imperforate anus
-
Myelodysplasia (tethered cord, myelomeningocele, hydromyelia, diastematomyelia)
-
Fetal uropathy with oligohydramnios and pulmonary hypoplasia
-
Compression abnormalities: Indented thorax, malformed digits, talipes (club foot), bowed limbs, and dislocated hips
-
Low-set ears
See the following images.
 Pediatric omphalocele and gastroschisis (abdominal wall defects). This photograph shows cloacal exstrophy in an infant.
Pediatric omphalocele and gastroschisis (abdominal wall defects). This photograph shows cloacal exstrophy in an infant.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). An intact omphalocele in an infant is shown.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This photograph depicts an umbilical cord hernia in an infant.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This intraoperative photograph reveals and infant with gastroschisis.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This intraoperative image reveals a ruptured omphalocele in an infant.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Gastroschisis and associated intestinal atresia is shown in an infant.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This intraoperative image reveals gastroschisis and colon atresia in an infant. The bulbous proximal end of the atretic colon is excised, and a colostomy is created at the abdominal wall defect. An anastomosis of the proximal, dilated colon to the distal microcolon (in view of its small caliber) would not function properly. The colostomy can be closed 4-6 weeks later.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Note the enlarged tongue in this infant with Beckwith-Wiedemann syndrome.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This infant has pentalogy of Cantrell: an epigastric omphalocele, cleft sternum, anterior (retrosternal) diaphragmatic hernia of Morgagni, absent pericardium, and cardiac defects (ectopia cordis, ventricular septal defects).
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This image demonstrates silo closure in an infant with gastroschisis.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Silon sheets are pulled over the omphalocele sac, elevating the rectus muscles, and, because of their attachment to the costal arch, expanding the thoracic cavity. The Silon sheets are removed and replaced by a permanent Gore-Tex patch that is covered by skin flaps.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This infant has a giant omphalocele that was treated with topical agents for several weeks. The omphalocele sac will absorb, leaving granulation tissue that gradually epithelializes.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). The omphalocele sac was adherent to the protuberant liver in an infant. It was covered with Gore-Tex so that gradual reduction could be effected.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). The Gore-Tex sheet is imbricated, gradually reducing the liver into the abdominal cavity: The rectus muscles are pulled over the liver. The skin and subcutaneous tissues become adherent to the Gortex; the next step is to freshen the wound margins (excise the skin edge and the exposed Gortex) and suture the composite layers together.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Final skin closure of the giant omphalocele was delayed because the baby developed respiratory distress. Unfortunately, the patch became infected and was removed. Later, bipedicled flank flaps were used to close the giant omphalocele, but reduction was lost.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Split-thickness skin grafts were applied to the flank wounds resulting from mobilization of the bipedicle flaps.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This infant has prune-belly syndrome.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Note the laxity of the abdominal wall in this infant with prune-belly syndrome.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This photograph shows cloacal exstrophy in an infant.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Note the bifid genitalia in this infant with cloacal exstrophy.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). In the repair of cloacal exstrophy, the cecal plate in the middle of the bifid bladder is excised and used to create an ostomy, and the bladder halves are approximated.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Closure of the bladder exstrophy is shown.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Bladder exstrophy and epispadias is shown in an infant. Note the appearance of the bladder mucosa, indicating chronic inflammation.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This is another view demonstrating the epispadias shown in the previous image.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This image reveals isolated epispadias in an infant.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). An intraoperative finding is a patent omphalomesenteric duct, which is being excised.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Closure of a giant omphalocele with an Alloderm patch is shown.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This image was obtained 2 months after implantation, revealing epithelialization of the Alloderm patch.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Eight months after implantation, epithelialization is nearly complete, but a huge ventral hernia has developed.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This image shows a giant omphalocele in an infant, in which the liver assumes an ectopic position in the epigastrium.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). In this infant, gastroschisis has been complicated by jejunal atresia and loss of the entire distal small bowel (the grey tissue).
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Following lysis of adhesions and tubularization of the viable, mesenteric portion of the proximal jejunum, the eviscerated viscera are reduced and the gastroschisis abdominal wall defect is closed.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). The radiograph shows the intestine following multiple serial transverse enteroplasty (STEP) procedures.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This infant has gastroschisis and colon atresia, with the proximal end open. An ostomy is brought out of the silo.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Inflammatory distortion of the extruded intestine is shown. There appears to be an associated atresia (the dilated intestine), but the dilatation resolved in concert with resolution of the inflammation.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). A silo is fashioned from Silon sheets, in case reduction of the extruded intestine cannot be achieved without unduly elevating the intra-abdominal pressure.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). The sac is removed, and the abdominal wall defect is closed around the in utero colostomy.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This infant had a small omphalocele sac whose contents were liver and gall bladder.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). The omphalocele sac contains liver and gall bladder.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). A completed repair is shown, simulating an umbilicus.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This child, approximately age 30 months in the photo, had a successful repair. Her clinical course is described above.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This image shows the appearance of the dilated bowel prior to performing the serial transverse enteroplasty (STEP) procedure.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This is the intestine as it appeared after the serial transverse enteroplasty (STEP) procedure.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This is the intestine as it appeared after the serial transverse enteroplasty (STEP) procedure.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This image shows an omphalomesenteric duct remnant presenting as an "umbilical granuloma."
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Rather than pushing the extruded viscera into the diminutive abdominal cavity, traction is applied to the abdominal wall and skin flaps. This stimulates growth and facilitates reduction of the extruded visceral and ultimate closure of the abdominal wall defect. Courtesy of Russell Jennings, MD, Boston Children's Hospital.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). This photograph depicts progress in reducing the extruded viscera utilizing Dr Jennings's innovative technique. Image courtesy of Russell Jennings, MD, Boston Children's Hospital.
-
Pediatric omphalocele and gastroschisis (abdominal wall defects). Reduction of the extruded viscera is gradually achieved. Courtesy of Russell Jennings, MD, Boston Children's Hospital.










