History
Cervicitis is often asymptomatic in gonorrhea, chlamydia, and T vaginalis infections. When present, symptoms are often nonspecific and may include increased vaginal discharge, dysuria, urinary frequency, and intermenstrual or postcoital bleeding. [1] If the infection has been long-standing, symptoms can include low abdominal or low back pain.
Most patients with herpes simplex virus (HSV) infection are asymptomatic. However, the first episode of genital herpes is frequently highly symptomatic and is marked by painful ulcerations associated with fever, myalgia, headache, and general malaise. Dysuria, vaginal discharge, and urethral discharge are also common symptoms. Recurrent outbreaks of HSV tend to be milder, but most patients have prodromal symptoms of itching or tingling, followed by the appearance of vesicles.
Because many causes of cervicitis are initially asymptomatic, ask all sexually active women for their complete gynecologic and sexual history at the initial evaluation and yearly thereafter.
In addition to the basic gynecologic history (eg, age of menarche, date of last menstrual period, gravida, para, pregnancy or delivery complications, date of last Papanicolaou test [Pap smear]), a complete sexual history is needed. This information includes the following:
-
Number of recent and current partners (in the last 3 mo)
-
Condom use
-
Non-barrier contraception use
-
Exchanging of sex for money or drugs
-
Previous diagnoses of sexually transmitted infections (STIs)
A focused review of symptoms is recommended that asks about the following:
-
Dyspareunia
-
Vaginal discharge
-
Genital skin lesions
-
Abnormal vaginal bleeding
-
Dysuria
-
Genital burning
-
Genital itching
-
Genital malodor
-
Lower abdominal or pelvic pain
Physical Examination
The physical examination should include a general survey, an external inspection, and pelvic speculum and bimanual examinations. In certain patients, a rectal examination should be performed.
The physical examination is crucial to the evaluation and diagnosis of cervicitis, but it should not be limited to the pelvic region. An assessment for lymphadenopathy, skin lesions, oral lesions, joint redness or swelling, abdominal pain, and costovertebral angle tenderness can point to disseminated infection.
The pelvic examination must be performed in a competent and sensitive manner. The presence of a nursing assistant is advised to help with the examination and to act as a chaperone. Always explain to the patient what is going to be done before proceeding. Begin with a neutral touch on the patient's thigh and visually investigate the external genitalia in good lighting. Note any skin lesions (eg, warts, ulcers, vesicles, excoriations, erythema), inflammation of the Bartholin or Skene glands, or inguinal lymphadenopathy.
Speculum examination
Perform the speculum examination with water or gel lubrication (eg, Surgilube or K-Y jelly), and include direct visualization of the vaginal walls and cervix. Remember that normal vaginal secretions are nonadherent to the vaginal walls, clear to white in color, and nonodorous. Normal vaginal secretions have an acidic pH of less than 4.5. Vaginitis is present if the vaginal discharge is copious, colored, and malodorous, or if the pH is greater than 4.5.
Cervicitis is suspected if the cervix is erythematous, edematous, or easily friable. Classic mucopurulent cervicitis is present if thick, yellow-green pus is visible in the endocervical canal (the cervical os) or on an endocervical swab specimen. Laboratory specimens are collected for study at this point. Note cervical warts or ulcerations.
Bimanual examination
After the speculum is removed, a bimanual examination is performed to assess tenderness or enlargement of the cervix, uterus, and adnexa. Cervicitis or pelvic inflammatory disease (PID) is suspected if the patient has cervical motion tenderness (ie, if she experiences pain or tenderness while the examiner gently moves the cervix from side to side).
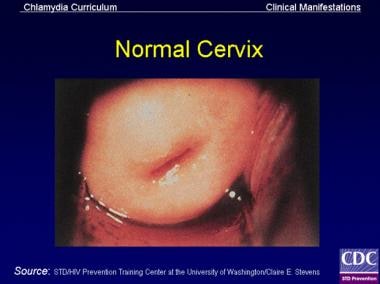
The following images depict a normal cervix, followed by images of cervicitis caused by various organisms.
 Cervix of a lactating woman without sexually transmitted infections. The patient had twice given birth vaginally.
Cervix of a lactating woman without sexually transmitted infections. The patient had twice given birth vaginally.
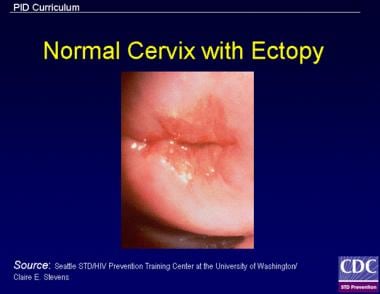 Cervical cellularity (ectopy), which is often present in adolescents, allows for greater adherence of infectious organisms in the cervix. The risk of acquiring acute salpingitis for a sexually active 15-year-old is 1:8, compared with 1:80 for women aged 24 years and older.
Cervical cellularity (ectopy), which is often present in adolescents, allows for greater adherence of infectious organisms in the cervix. The risk of acquiring acute salpingitis for a sexually active 15-year-old is 1:8, compared with 1:80 for women aged 24 years and older.
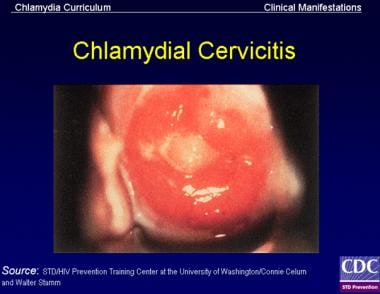 Signs of chlamydial cervicitis on speculum examination may include mucopurulent endocervical discharge and spontaneous or easily induced endocervical bleeding or any zones of ectopy.
Signs of chlamydial cervicitis on speculum examination may include mucopurulent endocervical discharge and spontaneous or easily induced endocervical bleeding or any zones of ectopy.
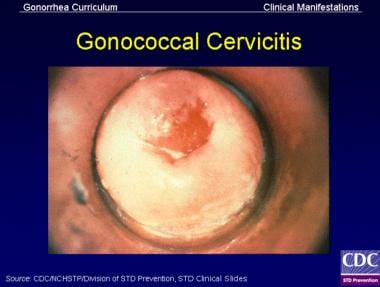 In women with gonococcal cervicitis, the cervix may show mucopurulent or purulent cervical discharge and easily induced cervical bleeding.
In women with gonococcal cervicitis, the cervix may show mucopurulent or purulent cervical discharge and easily induced cervical bleeding.
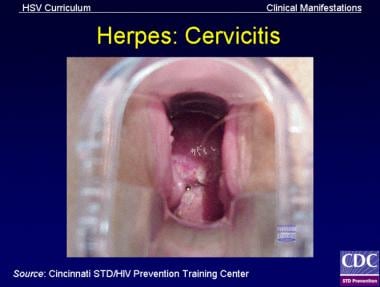 Herpes simplex virus (HSV) cervicitis may involve the exocervix or endocervix, and it may be symptomatic or asymptomatic. Usually, the cervix appears abnormal to inspection, with diffuse vesicular lesions, ulcerative lesions, erythema, or friability.
Herpes simplex virus (HSV) cervicitis may involve the exocervix or endocervix, and it may be symptomatic or asymptomatic. Usually, the cervix appears abnormal to inspection, with diffuse vesicular lesions, ulcerative lesions, erythema, or friability.
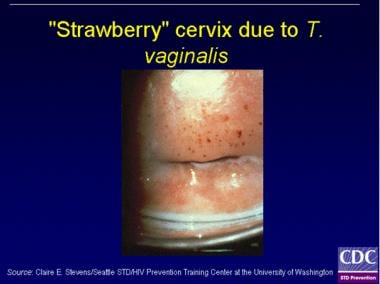 T vaginalis can have a characteristic "frothy" gray or yellow-green vaginal discharge and pruritus. The occurrence of cervical petechiae, or "strawberry cervix," is a classic presentation that is seen in less than 2% of cases. T vaginalis may also infect the Skene glands and the urethra and may be asymptomatic in women.
T vaginalis can have a characteristic "frothy" gray or yellow-green vaginal discharge and pruritus. The occurrence of cervical petechiae, or "strawberry cervix," is a classic presentation that is seen in less than 2% of cases. T vaginalis may also infect the Skene glands and the urethra and may be asymptomatic in women.
-
Normal cervix
-
Cervix of a lactating woman without sexually transmitted infections. The patient had twice given birth vaginally.
-
Cervical cellularity (ectopy), which is often present in adolescents, allows for greater adherence of infectious organisms in the cervix. The risk of acquiring acute salpingitis for a sexually active 15-year-old is 1:8, compared with 1:80 for women aged 24 years and older.
-
Signs of chlamydial cervicitis on speculum examination may include mucopurulent endocervical discharge and spontaneous or easily induced endocervical bleeding or any zones of ectopy.
-
In women with gonococcal cervicitis, the cervix may show mucopurulent or purulent cervical discharge and easily induced cervical bleeding.
-
Herpes simplex virus (HSV) cervicitis may involve the exocervix or endocervix, and it may be symptomatic or asymptomatic. Usually, the cervix appears abnormal to inspection, with diffuse vesicular lesions, ulcerative lesions, erythema, or friability.
-
T vaginalis can have a characteristic "frothy" gray or yellow-green vaginal discharge and pruritus. The occurrence of cervical petechiae, or "strawberry cervix," is a classic presentation that is seen in less than 2% of cases. T vaginalis may also infect the Skene glands and the urethra and may be asymptomatic in women.
-
Papanicolaou (Pap) stain, high power, showing the Herpes simplex virus (HSV) infecting cells with multiple nuclei, intranuclear inclusions, and margination of the chromatin to the outer portion of the nuclei.
-
Pap stain, high power, showing human papillomavirus (HPV) infecting a cell with a dark, wrinkled nucleus surrounded by a clear cytoplasmic halo.
-
Pap stain, high power (under oil immersion), showing 2 pear-shaped structures representing Trichomonas. Small, pale nuclei and cytoplasmic granules are present.