Definition
Testicular sex cord stromal tumors include Leydig cell tumors, Sertoli cell tumors, and granulosa cell tumors. Leydig cell tumors (see the image below) are derived from normal Leydig cells that produce testosterone and are located in the interstitium of the testis. [1, 2, 3]
A typical Sertoli cell tumor (see the images below) is a tumor derived from Sertoli cells, located within seminiferous tubules, which help support spermatogenesis. Sclerosing Sertoli cell tumor is a rare variant of the Sertoli cell tumor. Large-cell calcifying Sertoli cell tumor is also a rare variant of a Sertoli cell tumor. [4, 5, 6, 7]
Granulosa cells are not native to the testis. Adult-type granulosa cell tumors of the testicle are much less common than in the adult female ovary. The juvenile type of this condition is a rare sex cord stromal tumor that occurs in males in the first few months of life. [8]
Epidemiology
Leydig cell tumors constitute about 3% of testicular neoplasms and occur in both adults (80% of cases) and children. Sertoli cell tumors account for less than 1% of testicular tumors, and they occur both in children (15% of cases) and in middle-aged adults and can be malignant (about 10% of cases) in both. [4, 9, 10]
Clinical Features and Imaging
Leydig cell tumor
Boys with Leydig cell sex cord stromal tumors present with endocrinologic symptoms (virilization, gynecomastia), while men present with a testicular mass; some (10-30%) have gynecomastia. In boys, Leydig cell tumors are benign. However, in men, 10-17% of these tumors are malignant. Tumors are unilateral, with rare exceptions.
Sertoli cell tumor
Patients with Sertoli cell sex cord stromal tumors present with a testicular mass, and estrogen production by the tumor can result in gynecomastia and impotence. The treatment is orchiectomy. Estrogens secreted by the Sertoli cells may promote the female phenotype. In sclerosing Sertoli cell tumor, patients present with a testicular mass and without endocrinologic symptoms. No malignant cases have been reported.
In large-cell calcifying Sertoli cell tumor, patients are young, with age at diagnosis ranging from 16-37 years. The tumor occurs both as a part of the Carney complex and in patients with Peutz-Jeghers syndrome. In this setting, the tumor tends to be multifocal.
Malignant tumors may occur and are usually sporadic (with one report of a malignant tumor associated with Carney syndrome). [4]
Granulosa cell tumor
In patients with granulosa cell tumor, the average age is 42 years, and 20% of male patients present with gynecomastia. Of 4 patients reported with metastasis, 2 died.
Gross Findings
Leydig cell tumor
Leydig cells impart a yellow to yellow-tan color; the tumor is solid and lobulated. Malignant tumors tend to be larger (>5 cm) than benign tumors. Necrosis can be seen in malignant tumors.
Sertoli cell tumor
Tumors are well-circumscribed, solid-pale-yellow, or white-to-gray masses. Large size and necrosis are worrisome features for malignancy. Sclerosing Sertoli cell tumor is similar to a typical Sertoli cell tumor. In large-cell calcifying Sertoli cell tumor, benign tumors are small (usually < 2 cm), yellow, tan, or white nodules confined to the testicle. Malignant tumors are larger and may have areas of necrosis.
Granulosa cell tumor
The mass is lobulated, firm, and uniformly yellow-gray. Tumors of the juvenile type are small and solid and contain multiple small cysts.
Microscopic Findings
Leydig cell tumor
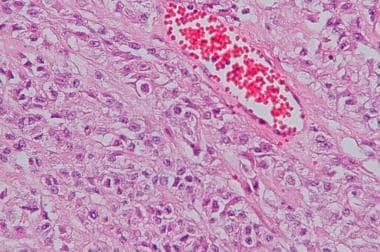
Leydig cells vary in size but usually have round nuclei, single prominent nucleoli, and abundant eosinophilic cytoplasm or abundant clear cytoplasm (see the image below). [11, 12, 13] Reinke crystals are present in 40-70% of cases, and lipochrome can be abundant in some cases. Electron microscopy shows mitochondria with tubular cristae. Rarely, adipose differentiation or spindle cell growth is noted.
Malignant features include large size (>5 cm), increased mitotic activity (>5/10 hpf), necrosis, angiolymphatic invasion, and invasion of surrounding structures, such as tunica, epididymis, and spermatic cord. Malignant behavior is difficult to predict based on histologic features.
These tumors do not respond to radiation; thus, the differential diagnosis with seminoma is crucial. Lack of inhibin-alpha reactivity suggests a germ cell tumor. Differential diagnosis includes testicular tumor of adrenogenital syndrome, which is bilateral, dark brown grossly, and, less often, immunoreactive with inhibin-alpha. Leydig cell hyperplasia is multifocal rather than forming a single mass and does not efface seminiferous tubules.
Sertoli cell tumor
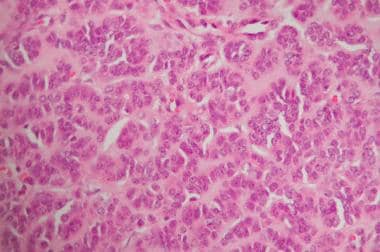
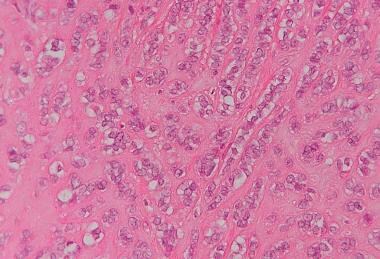
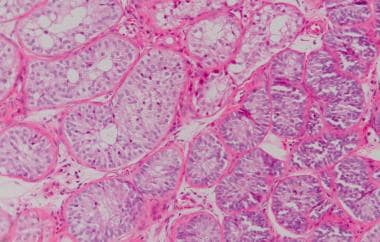
Sertoli cell tumors are typically composed of solid tubules containing Sertoli cells. [11, 12, 13] Tubules can contain lumina. Also, cells may be arranged in cords (see the first image below), solid nests, and sheets. By electron microscopy, Charcot-Bottcher filaments (perinuclear aggregates of intermediate filaments) are pathognomonic of Sertoli cells or Sertoli cell differentiation. In sclerosing Sertoli cell tumor, cords, nests, and tubules of Sertoli cells are present within a fibrotic stroma (see the second image below).
Malignant behavior can be difficult to predict. Features worrisome for malignancy are identical to those seen in Leydig cell tumors.
In large-cell calcifying Sertoli cell tumor, neoplastic cells are arranged in sheets, small nests, and cords, and they are present in a myxoid to fibrous stroma. Dystrophic calcifications, including psammomatous calcifications, are present. Malignant tumors are large and exhibit extratesticular spread, increased mitotic activity, necrosis, and angiolymphatic invasion.
The proliferation of Sertoli cells may also be seen in androgen insensitivity syndrome in XY male patients with male, female, or ambiguous phenotype (“tubular adenoma” or Sertoli cell adenoma; see the first image below) and in the cryptorchid testis (Sertoli cell nodule or Pick adenoma; see the second image below). Malignant cases are often misinterpreted as seminoma, and immunostains may help. [14]
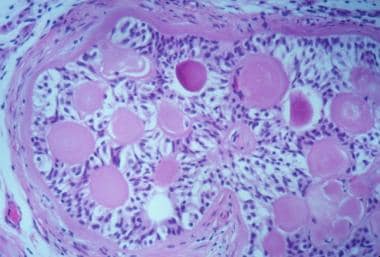 Sertoli cell adenoma with central laminated deposits in some tubules. Courtesy of Dr. W.M. Murphy, Gainesville, FL.
Sertoli cell adenoma with central laminated deposits in some tubules. Courtesy of Dr. W.M. Murphy, Gainesville, FL.
 Sertoli cell nodule (right) or Pick adenoma, within cryptorchid testis, in which tubules show aspermatogenesis (left). Courtesy of Kenneth A. Iczkowski, MD.
Sertoli cell nodule (right) or Pick adenoma, within cryptorchid testis, in which tubules show aspermatogenesis (left). Courtesy of Kenneth A. Iczkowski, MD.
Granulosa cell tumor
Granulosa cell tumor is microfollicular with a few larger cysts. Call-Exner bodies may be seen. Cells have scant cytoplasm and angular nuclei. They may have nuclear grooves. The juvenile type has sheets of spindle cells with abundant cytoplasm intermixed with follicle-like cystic spaces. Hyalinized collagenous stroma is also a feature in cellular areas. [15]
Immunohistochemistry
Leydig cell tumor
Inhibin-alpha is reactive in 100% of cases. [12] The tumor shows variable reactivity with cytokeratins and rarely reacts with S-100 protein, chromogranin, synaptophysin, and estrogen and progesterone receptors.
Sertoli cell tumor
Inhibin-alpha is a specific marker, but Sertoli cell tumors are less consistently reactive than Leydig cell tumors (91% in Iczkowski’s series, but 47% of cases in combined series). [12] Tumors can be positive for synaptophysin, chromogranin, and S-100 protein and with cytokeratin AE1/3 and CAM5.2 in 64-100% of cases. [16]
In large-cell calcifying Sertoli cell tumor, S-100 is positive, EMA is negative, and cytokeratin is variable (usually negative to weak staining).
Tumor Spread and Staging
Staging for testicular sex cord stromal tumors is the same as for germ cell tumors.
-
Leydig cell tumor. Note the clear cytoplasm. Courtesy of Kenneth A. Iczkowski, MD.
-
Sertoli cell tumor with characteristic arrangement in cords. Courtesy of Kenneth A. Iczkowski, MD.
-
Sclerosing Sertoli cell tumor retains cord arrangement. Courtesy of Kenneth A. Iczkowski, MD.
-
Sertoli cell adenoma with central laminated deposits in some tubules. Courtesy of Dr. W.M. Murphy, Gainesville, FL.
-
Sertoli cell nodule (right) or Pick adenoma, within cryptorchid testis, in which tubules show aspermatogenesis (left). Courtesy of Kenneth A. Iczkowski, MD.