Approach Considerations
Evaluating children with infantile spasms for possible tuberous sclerosis is critical, as this is the single most common disorder, accounting for 10-30% of prenatal cases of infantile spasm. Tuberosis sclerosis is an autosomally dominant inherited disease with variable manifestations, including cardiac tumors, kidney tumors, cutaneous malformations such as ash-leaf hypopigmented lesions, and seizures.
In more than a few patients, the family diagnosis of tuberous sclerosis is found only after a child presents with infantile spasms, and an extensive workup of the child and, subsequently, the family reveals the genetic disease. Two-thirds of patients with tuberous sclerosis have a de novo mutation.
Lab studies
Prior to initiating therapy, consider obtaining some or all of the following laboratory studies:
-
Complete blood count (CBC) with differential, liver panel, renal panel with electrolytes and glucose, calcium, magnesium, phosphorus, and urinalysis with microscopic examination
-
Metabolic workup, including glucose, liver panel, serum lactate and pyruvate, plasma ammonia, serum and urine amino acids, urine organic acids, and serum biotinidase
-
Blood, urine, and cerebrospinal fluid cultures if an infection is suspected
-
Cerebrospinal fluid analysis for cell count, glucose, protein, bacterial and viral culture, lactate, pyruvate, and amino acids
Lumbar puncture
In young infants with early onset of infantile spasms, consider a lumbar puncture as part of a full sepsis workup to look for signs of meningitis.
In older infants in whom no clear signs of infection are present, a lumbar puncture is useful in evaluating metabolic causes of infantile spasms, such as nonketotic hyperglycinemia.
CT Scanning and MRI
About 70-80% of patients have abnormal findings on neuroimaging studies. Magnetic resonance imaging (MRI) of the brain provides a more detailed evaluation than does computed tomography (CT) scanning of the brain. Imaging studies should be obtained prior to starting ACTH or steroid therapy, as these therapies are associated with the appearance of apparent brain atrophy as treatment continues.
CT scanning
Structural brain anomalies such as hydrocephalus, hydranencephaly, schizencephaly, and agenesis of the corpus callosum can be recognized easily by CT scans.In addition, cerebral calcifications can be observed in patients with tuberous sclerosis or congenital infections. However, unless CT is indicated to assess for an acute process, MRI is preferred due to greater detail and lack of radiation exposure.
MRI
MRI scans are superior to CT scans in detecting areas of cortical dysgenesis, disorders of neuronal migration, or disorders of myelination.
Electroencephalography
Always perform an EEG in patients with suspected infantile spasms, since the diagnosis depends on the presence of specific EEG findings. [12]
If possible, obtain prolonged video-EEG telemetry to record waking and sleeping EEG to assist in confirming a suspected diagnosis. A routine 20-minute EEG may not capture the patient while both awake and asleep and thus may miss specific important EEG findings. If there are no interictal abnormalities, prolonged video-EEG to catch the events of concern would also assist in differentiating them from other movements such as benign myoclonus of infancy.
Interictal electroencephalogram
Hypsarrhythmia (seen in the image below) is the characteristic interictal EEG pattern. It consists of chaotic, high- to extremely high–voltage, polymorphic delta and theta rhythms with superimposed multifocal spikes and wave discharges. Multiple variations of this pattern are possible, including focal or asymmetrical hypsarrhythmia.
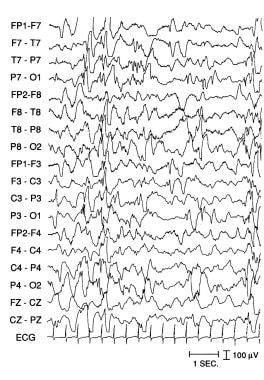 Mountainous, chaotic, disorganized rhythms with superimposed multifocal spikes demonstrating hypsarrhythmia in a boy aged 8 months with infantile spasms and developmental delay. Courtesy of E Wyllie.
Mountainous, chaotic, disorganized rhythms with superimposed multifocal spikes demonstrating hypsarrhythmia in a boy aged 8 months with infantile spasms and developmental delay. Courtesy of E Wyllie.
In a study of 77 patients with infantile spasms, unilateral hypsarrhythmia and asymmetrical ictal EEG changes during spasms often occurred together and correlated with focal or asymmetrical cerebral lesions on imaging studies. Patients with symmetrical hypsarrhythmia and infantile spasms rarely had focal or asymmetrical cerebral lesions on imaging studies (most had structural diffuse brain lesions), and overall they had better chances for a normal outcome.
In a study of 26 patients with infantile spasms, 6 patients (23%) had asymmetrical hypsarrhythmia. All 6 had symptomatic infantile spasms and 5 had focal abnormalities on examination or imaging study (4 ipsilateral to the lesion, 1 contralateral). These focal abnormalities may identify a subset of patients with infantile spasms who are candidates for focal cortical resections.
Ictal electroencephalogram
Eleven different types of ictal patterns have been identified in patients with infantile spasms. In one study, the most common pattern, found in 38% of patients with seizures, was a high-voltage, frontal dominant, generalized slow-wave transient followed by voltage attenuation, also termed an electrodecremental episode. These electrodecremental episodes were a feature in 71% of the seizures.No close correlation exists between the type of seizure and the EEG pattern.
-
Mountainous, chaotic, disorganized rhythms with superimposed multifocal spikes demonstrating hypsarrhythmia in a boy aged 8 months with infantile spasms and developmental delay. Courtesy of E Wyllie.







